Respiratory System
Breathe Easy: A Comprehensive Guide to Understanding the Respiratory System
The respiratory system is a vital biological system responsible for the exchange of gases between an organism and its environment. In humans, this intricate network of organs and tissues facilitates breathing, allowing us to take in oxygen, crucial for cellular function, and expel carbon dioxide, a waste product of metabolism. Understanding the respiratory system is not just an academic pursuit; it's fundamental to comprehending human health, disease, and the very essence of life. For those considering a career related to this field, or simply curious individuals, a journey into the world of the respiratory system offers a fascinating glimpse into the mechanics of our bodies.
Exploring the respiratory system can be deeply engaging. Imagine the elegance of how our lungs, like bellows, draw in air, and how, at a microscopic level, tiny air sacs called alveoli perform the life-sustaining swap of oxygen for carbon dioxide. Consider the excitement of contributing to medical advancements that help people breathe easier, whether through developing new therapies for asthma or designing innovative life-support equipment. The field also offers the satisfaction of directly impacting patient well-being, a rewarding aspect for those drawn to healthcare professions. Furthermore, understanding the respiratory system connects to broader environmental and societal issues, such as the impact of air quality on public health.
Introduction to the Respiratory System
A grasp of the respiratory system is more than just learning about lungs; it's about understanding a cornerstone of biological life. This section will introduce the fundamental concepts, its connections to other bodily functions, some historical context, and its relevance in today's world, especially concerning environmental factors that impact our breathing.
Definition and Primary Functions
The respiratory system is a complex network of organs and tissues whose primary function is to enable gas exchange. This means it's responsible for bringing oxygen into the body, which is essential for cells to produce energy, and removing carbon dioxide, a waste product of this energy production. Think of it as the body's air-filtration and gas-delivery service. Beyond this core role, the respiratory system also contributes to other important functions like vocalization (speech), regulating blood pH by managing carbon dioxide levels, and providing a defense against inhaled pathogens and irritants through mechanisms like coughing and the mucociliary escalator.
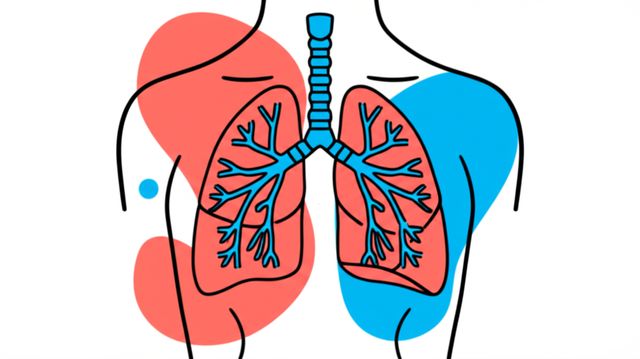
The process begins when you inhale air through your nose or mouth. The air then travels down the pharynx (throat) and larynx (voice box) into the trachea (windpipe). The trachea branches into two main bronchi, one for each lung. These bronchi further divide into smaller and smaller tubes called bronchioles, eventually leading to tiny air sacs known as alveoli. It is within these millions of alveoli that the magic of gas exchange occurs: oxygen from the inhaled air diffuses into the blood, while carbon dioxide from the blood diffuses into the alveoli to be exhaled.
This system doesn't just passively move air; it also conditions it. As air passes through the nasal passages and upper airways, it is warmed, humidified, and filtered to remove dust and other particles. This preparation helps protect the delicate tissues of the lower respiratory tract. The entire process is a marvel of biological engineering, ensuring that every cell in your body receives the oxygen it needs to survive and function.
Relationship to Other Bodily Systems
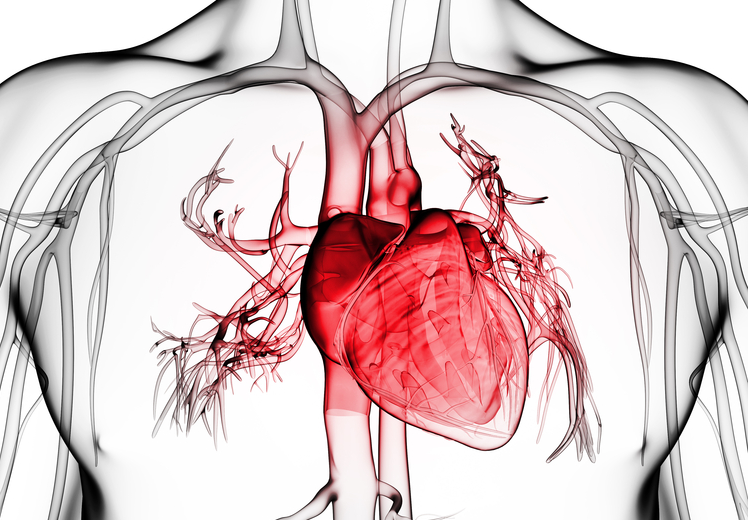
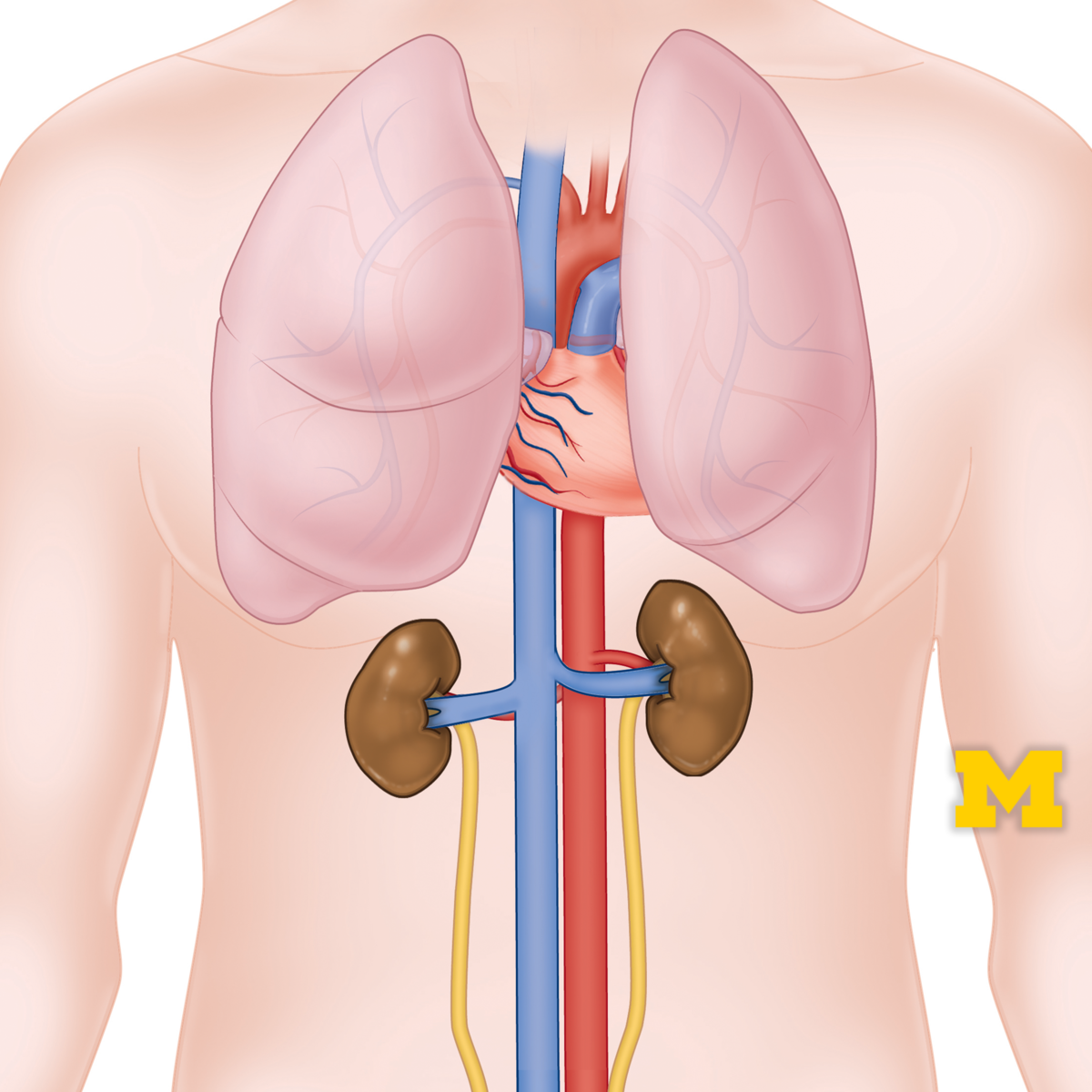
The respiratory system does not operate in isolation; it is intricately linked with several other bodily systems, most notably the cardiovascular system. This partnership is so critical that they are often referred to together as the cardiopulmonary system. The respiratory system is responsible for bringing oxygen into the body and removing carbon dioxide, while the cardiovascular system, through the heart and blood vessels, transports these gases to and from the cells. Oxygen picked up by the blood in the lungs is carried by red blood cells to tissues throughout thebody, and carbon dioxide produced by these tissues is transported back to the lungs for exhalation.
The nervous system also plays a crucial role in controlling respiration. The brainstem, specifically the medulla oblongata and pons, regulates the rate and depth of breathing automatically, even when we are not consciously thinking about it. Sensory receptors throughout the body monitor oxygen, carbon dioxide, and pH levels in the blood, sending signals to the brain to adjust breathing as needed. For instance, during exercise, as muscles consume more oxygen and produce more carbon dioxide, the nervous system signals the respiratory muscles to increase the breathing rate and depth.
Furthermore, the respiratory system interacts with the immune system to protect against inhaled pathogens. The airways are lined with mucus and cilia, which trap and remove foreign particles. Immune cells are also present in the lung tissue to fight off infections. The musculoskeletal system, particularly the diaphragm and intercostal muscles, provides the mechanical force needed for breathing. These interconnections highlight the holistic nature of bodily functions, where each system relies on others to maintain overall health and homeostasis.
These courses provide a foundational understanding of human physiology, including how the respiratory system interacts with other body systems.
Historical Discoveries in Respiratory Science
The understanding of the respiratory system has evolved significantly over centuries, built upon the observations and experiments of numerous scientists and physicians. Ancient civilizations had rudimentary ideas about breathing, often linking it to life force or spirit, but the intricate mechanics remained a mystery. Early Greek philosophers like Empedocles and later physicians such as Galen made some of the first recorded observations, though their theories were often based on speculation rather than empirical evidence. Galen, for example, believed that the lungs cooled the heart and that air was transformed into a "vital spirit" in the left ventricle.
The Renaissance brought a renewed interest in human anatomy. Leonardo da Vinci's detailed anatomical drawings, including those of the lungs and airways, marked a significant step forward. However, a more scientific understanding began to emerge in the 17th and 18th centuries. Scientists like Robert Boyle described the relationship between pressure and volume of gases (Boyle's Law), fundamental to understanding the mechanics of breathing. Joseph Black, Antoine Lavoisier, and Joseph Priestley were pivotal in discovering and understanding gases like carbon dioxide and oxygen, and Lavoisier is credited with demonstrating that respiration is a form of slow combustion where oxygen is consumed and carbon dioxide is produced.
The 19th and 20th centuries saw rapid advancements. The invention of the stethoscope by René Laennec allowed for better diagnosis of lung diseases. The development of microscopy enabled detailed study of lung tissues and the alveoli. Figures like John Hutchinson developed the spirometer to measure lung volumes, a tool still crucial today. The understanding of gas exchange at the alveolar-capillary membrane, oxygen and carbon dioxide transport in the blood (including the role of hemoglobin), and the neural control of breathing were progressively elucidated. These historical milestones have paved the way for modern respiratory medicine and continue to inspire further research.
Societal Relevance (e.g., Air Pollution Impacts)
The respiratory system's health is profoundly impacted by the environment, making its study highly relevant to societal concerns, particularly air pollution. Air pollution, stemming from industrial emissions, vehicle exhaust, wildfires, and indoor sources like tobacco smoke and cooking fuels, poses a significant global health threat. According to the World Health Organization (WHO), almost all of the global population (99%) breathes air that exceeds WHO guideline limits, containing high levels of pollutants. The combined effects of ambient (outdoor) and household air pollution are associated with millions of premature deaths annually.
Pollutants such as particulate matter (PM2.5 and PM10), nitrogen dioxide (NO2), sulfur dioxide (SO2), ozone (O3), and volatile organic compounds (VOCs) can penetrate deep into the lungs and even enter the bloodstream, causing a range of health problems. Short-term exposure can trigger asthma attacks, worsen chronic bronchitis, and increase susceptibility to respiratory infections. Long-term exposure is linked to the development of chronic respiratory diseases like Chronic Obstructive Pulmonary Disease (COPD) and lung cancer, as well as cardiovascular diseases. Children, the elderly, and individuals with pre-existing lung or heart conditions are particularly vulnerable to the detrimental effects of air pollution.
Addressing air pollution requires a multi-faceted approach involving policy changes, technological innovation, and public awareness. Understanding the mechanisms by which pollutants affect the respiratory system is crucial for developing effective interventions and public health strategies. This includes research into better air quality monitoring, the development of protective measures, and advocacy for cleaner energy sources and sustainable urban planning. The societal relevance of respiratory science thus extends beyond medicine into environmental policy, public health, and engineering, highlighting the interconnectedness of human health and the environment. You can learn more about the global impact from resources provided by the World Health Organization.
Anatomy of the Respiratory System
To truly understand how we breathe and why things can go wrong, a detailed look at the structure, or anatomy, of the respiratory system is essential. This section delves into the specific components, from the larger airways to the microscopic gas-exchanging units, and even touches on how our breathing apparatus compares to that of other creatures.
Upper vs. Lower Respiratory Tract Structures
The respiratory system is broadly divided into two main sections: the upper respiratory tract (URT) and the lower respiratory tract (LRT). The URT primarily serves as a passageway for air and also plays roles in filtering, warming, and humidifying the air before it reaches the delicate tissues of the LRT. Structures of the URT include the nose and nasal cavity, paranasal sinuses, the pharynx (throat), and the portion of the larynx (voice box) above the vocal cords. The nasal cavity is lined with hairs and mucus-producing cells that trap larger particles, while its rich blood supply helps warm the inhaled air. The sinuses, air-filled spaces within the skull bones, also contribute to warming and humidifying air and can affect voice resonance.
The pharynx is a muscular funnel that extends from the base of the skull to the beginning of the esophagus and trachea. It serves as a common pathway for both air and food. It is divided into three regions: the nasopharynx (behind the nasal cavity), the oropharynx (behind the oral cavity), and the laryngopharynx (the inferior part, leading to the larynx and esophagus). The larynx, or voice box, sits below the pharynx and houses the vocal cords, which produce sound when air passes over them. It also plays a crucial role in preventing food from entering the lower airways via a flap-like structure called the epiglottis.
The lower respiratory tract begins with the trachea (windpipe) and includes all structures within the lungs. The trachea is a cartilaginous tube that extends from the larynx and bifurcates (divides) into the right and left main bronchi. These main bronchi enter the lungs and continue to divide into progressively smaller airways: lobar bronchi (to each lobe of the lung), segmental bronchi, and then numerous generations of smaller bronchioles. The terminal bronchioles lead to the respiratory bronchioles, alveolar ducts, alveolar sacs, and finally, the alveoli, which are the primary sites of gas exchange. The lungs themselves are paired, cone-shaped organs located in the thoracic cavity, protected by the rib cage.
These courses offer detailed explorations of the anatomical structures of the respiratory system.
Alveoli and Gas Exchange Mechanisms
The alveoli are the functional units of the lungs, tiny, balloon-like sacs where the critical process of gas exchange occurs. There are hundreds of millions of alveoli in the human lungs, providing an immense surface area for this exchange – roughly the size of a tennis court if spread out. Each alveolus is surrounded by a dense network of capillaries, which are tiny blood vessels. The walls of both the alveoli and the capillaries are extremely thin, typically only one cell thick, forming what is known as the respiratory membrane or alveolar-capillary membrane.
Gas exchange happens through a process called simple diffusion. This means that gases move from an area of higher concentration (or partial pressure) to an area of lower concentration. When you inhale, the air filling the alveoli has a high concentration of oxygen and a low concentration of carbon dioxide. Conversely, the blood arriving in the pulmonary capillaries from the body's tissues has a low concentration of oxygen (as it has been used by the cells) and a high concentration of carbon dioxide (a waste product of cellular metabolism). Due to these concentration gradients, oxygen diffuses from the alveoli across the respiratory membrane into the blood in the capillaries, where it binds to hemoglobin in red blood cells. Simultaneously, carbon dioxide diffuses from the blood in the capillaries across the respiratory membrane into the alveoli, from where it can be expelled from the body during exhalation.
The efficiency of this gas exchange is remarkable. Several factors contribute to this efficiency, including the vast surface area provided by the millions of alveoli, the thinness of the respiratory membrane minimizing the diffusion distance, and the close matching of airflow (ventilation) to blood flow (perfusion) in the lungs. The inner surface of the alveoli is also lined with a thin layer of fluid containing surfactant, a substance that reduces surface tension and prevents the alveoli from collapsing, making it easier for them to inflate with each breath.
For a deeper understanding of these intricate processes, "West's Respiratory Physiology" is a highly regarded text.
Another excellent resource that covers these topics comprehensively is "Pulmonary Physiology, Seventh Edition."
Muscles Involved in Breathing
Breathing, or ventilation, is a mechanical process driven by the coordinated action of several muscles. The primary muscle of inspiration (inhalation) is the diaphragm, a large, dome-shaped muscle located at the base of the chest cavity, separating the thorax from the abdomen. When the diaphragm contracts, it flattens and moves downward, increasing the vertical dimension of the thoracic cavity. Simultaneously, the external intercostal muscles, located between the ribs, contract, pulling the rib cage upward and outward. This combined action expands the volume of the thoracic cavity.
According to Boyle's Law, if the volume of a container increases, the pressure inside it decreases (assuming temperature remains constant). So, as the thoracic cavity expands, the pressure within the lungs (intrapulmonary pressure) drops below atmospheric pressure. This pressure difference causes air to flow from the higher pressure outside the body into the lower pressure inside the lungs, resulting in inhalation. Normal, quiet exhalation, on the other hand, is largely a passive process. It occurs when the diaphragm and external intercostal muscles relax. The natural elasticity of the lungs and chest wall causes them to recoil, decreasing the volume of the thoracic cavity. This decrease in volume increases the intrapulmonary pressure above atmospheric pressure, forcing air out of the lungs.
During forceful breathing, such as during strenuous exercise or when experiencing respiratory distress, accessory muscles are recruited to assist with both inhalation and exhalation. Accessory muscles of inhalation include the sternocleidomastoid and scalene muscles in the neck, and the pectoralis minor muscles in the chest; these help to further elevate the rib cage. Accessory muscles of exhalation include the internal intercostal muscles, which pull the ribs downward and inward, and the abdominal muscles (such as the rectus abdominis and obliques), which contract to push the diaphragm upward, forcefully decreasing thoracic volume and expelling air more rapidly.
This course provides a good overview of how different body systems, including the muscles involved in respiration, function.
Comparative Anatomy (e.g., Human vs. Avian Systems)
Studying the respiratory systems of different animal groups reveals fascinating adaptations to diverse environments and metabolic needs. While the fundamental goal of gas exchange is universal, the structures and mechanisms can vary significantly. For example, insects have a tracheal system, a network of air-filled tubes (tracheae) that branch throughout the body, delivering oxygen directly to tissues without the need for a circulatory system to transport gases. Fish, living in an aquatic environment, utilize gills, which are highly efficient at extracting dissolved oxygen from water through a countercurrent exchange mechanism.
The avian (bird) respiratory system is remarkably different from the mammalian system and is considered one of the most efficient among air-breathing vertebrates, supporting the high metabolic demands of flight. Birds possess relatively small, rigid lungs that do not expand and contract like mammalian lungs. Instead, they have a series of air sacs (typically nine) that extend into the body cavity and even into bones. Airflow in birds is unidirectional, meaning air passes through the lungs in a single direction, unlike the tidal (in-and-out) flow in mammals. This is achieved through a two-cycle breathing process. During the first inhalation, air passes through the trachea, mostly bypassing the lungs and filling the posterior air sacs. During the first exhalation, this air moves from the posterior air sacs into the lungs (parabronchi, where gas exchange occurs). With the second inhalation, oxygen-depleted air moves from the lungs into the anterior air sacs, while fresh air refills the posterior air sacs. Finally, during the second exhalation, air from the anterior air sacs is expelled, and air from the posterior air sacs moves into the lungs.
This unidirectional flow, coupled with a cross-current exchange system in the parabronchi, allows for more efficient oxygen extraction from the air compared to the mammalian system. In contrast, human lungs operate with a tidal flow, where air enters and exits through the same pathways, resulting in some mixing of fresh and "old" air (residual volume). Understanding these comparative aspects not only enriches our knowledge of biology but can also provide insights into physiological principles and potential inspirations for engineering solutions, such as in the design of medical ventilators or air filtration systems.
Respiratory System Physiology
Physiology delves into the functions and processes of living organisms. For the respiratory system, this means exploring how we actually breathe, how gases are transported throughout the body, how our breathing is controlled, and how the system adapts to challenging conditions. This section moves beyond structures to the dynamic actions that keep us alive.
Mechanics of Inhalation/Exhalation
The mechanics of breathing, also known as ventilation, involve the movement of air into and out of the lungs. This process is governed by pressure differences between the atmosphere and the alveoli, created by changes in the volume of the thoracic cavity. As previously touched upon, inhalation (inspiration) is an active process initiated by the contraction of the diaphragm and external intercostal muscles. The diaphragm flattens and descends, while the external intercostals lift the rib cage up and out. These actions increase the volume of the thoracic cavity.
This expansion of the chest wall also pulls the lungs outward, due to the adherence of the visceral pleura (covering the lungs) to the parietal pleura (lining the chest cavity), with a thin layer of pleural fluid in between creating surface tension. As lung volume increases, the pressure inside the lungs (intrapulmonary pressure) drops to about 1-3 mmHg below atmospheric pressure. This negative pressure gradient drives air into the lungs until intrapulmonary pressure equals atmospheric pressure. Intrapleural pressure, the pressure within the pleural cavity, is always negative relative to atmospheric pressure (about -4 mmHg at rest), acting like a suction to keep the lungs inflated and prevent them from collapsing.
Quiet exhalation (expiration) is typically a passive process, relying on the elastic recoil of the lungs and chest wall once the inspiratory muscles relax. As these structures return to their resting positions, the volume of the thoracic cavity decreases, causing the intrapulmonary pressure to rise about 1-3 mmHg above atmospheric pressure. This positive pressure gradient forces air out of the lungs. Forceful exhalation, however, is an active process involving the contraction of accessory muscles like the internal intercostals and abdominal muscles, which further reduce thoracic volume and expel air more vigorously and completely. Factors like airway resistance (affected by the diameter of the airways) and lung compliance (the ease with which lungs can be stretched) also play significant roles in the mechanics of breathing.
To delve deeper into the functional aspects of the respiratory system, "Respiratory Care Anatomy and Physiology" provides a comprehensive overview.
The course "Anatomy & Physiology: Exchange and Energy" also covers these physiological mechanisms.
Oxygen-CO₂ Transport in Blood
Once oxygen diffuses from the alveoli into the pulmonary capillary blood, it needs to be transported efficiently to all the tissues of the body. Similarly, carbon dioxide produced by cellular metabolism must be transported from the tissues back to the lungs for excretion. Blood serves as the transport medium for these gases. Oxygen is primarily transported in the blood bound to hemoglobin, a protein found within red blood cells. Each hemoglobin molecule can bind up to four oxygen molecules, forming oxyhemoglobin. This binding is reversible and depends on the partial pressure of oxygen (PO₂). In the lungs, where PO₂ is high, oxygen readily binds to hemoglobin. In the tissues, where PO₂ is lower due to cellular oxygen consumption, oxygen dissociates from hemoglobin and diffuses into the cells. Only a small fraction of oxygen (about 1.5-3%) is transported dissolved directly in the blood plasma because oxygen has low solubility in water.
Carbon dioxide (CO₂) is transported in the blood in three main forms. About 7-10% is dissolved directly in the plasma. Another 20-23% binds to hemoglobin (to the globin protein part, not the heme iron where oxygen binds), forming carbaminohemoglobin. The majority of CO₂, about 70%, is transported as bicarbonate ions (HCO₃⁻) in the plasma. This conversion occurs within red blood cells, where CO₂ combines with water in a reaction catalyzed by the enzyme carbonic anhydrase to form carbonic acid (H₂CO₃). Carbonic acid then quickly dissociates into hydrogen ions (H⁺) and bicarbonate ions (HCO₃⁻). The bicarbonate ions are then transported out of the red blood cells into the plasma in exchange for chloride ions (Cl⁻), a process known as the chloride shift. The hydrogen ions produced are buffered by hemoglobin.
In the lungs, these processes are reversed. Due to the lower partial pressure of CO₂ (PCO₂) in the alveoli, bicarbonate ions re-enter the red blood cells, combine with hydrogen ions to form carbonic acid, which then dissociates into CO₂ and water. Carbaminohemoglobin also releases its CO₂, and the dissolved CO₂ diffuses from the blood into the alveoli to be exhaled. The efficiency of these transport mechanisms is crucial for maintaining appropriate oxygen delivery to tissues and removal of CO₂ waste, thereby supporting cellular respiration and overall homeostasis.
The following course details the role of the respiratory system in gas exchange and transport, providing valuable insights into these mechanisms.
Neural Control of Breathing
The rhythmic pattern of breathing is generated and controlled by complex neural circuits located primarily in the brainstem, specifically in the medulla oblongata and pons. These respiratory centers ensure that ventilation is appropriately matched to the body's metabolic demands, even without conscious effort. The medulla contains two main groups of neurons: the dorsal respiratory group (DRG) and the ventral respiratory group (VRG). The DRG is primarily responsible for initiating inspiration. It sends signals via the phrenic nerve to the diaphragm and via intercostal nerves to the external intercostal muscles, causing them to contract.
The VRG contains neurons that are active during both inspiration and expiration, particularly during forceful breathing. Some neurons in the VRG contribute to augmenting inspiratory drive, while others are involved in active expiration by stimulating the internal intercostal and abdominal muscles. The pons also plays a role in modulating breathing, with two main centers: the pneumotaxic center and the apneustic center. The pneumotaxic center helps to fine-tune the breathing rhythm and is thought to limit the duration of inspiration, thereby influencing respiratory rate. The apneustic center appears to promote inspiration, but its exact role is less clear and is often overridden by signals from the pneumotaxic center.
Beyond this automatic control, breathing can also be influenced by various factors and inputs. Chemoreceptors are critical sensors that monitor the chemical composition of the blood and cerebrospinal fluid. Central chemoreceptors in the medulla are highly sensitive to changes in the partial pressure of carbon dioxide (PCO₂) and pH (hydrogen ion concentration) in the cerebrospinal fluid. Peripheral chemoreceptors, located in the carotid bodies (at the bifurcation of the common carotid arteries) and aortic bodies (in the aortic arch), primarily sense changes in blood PCO₂, pH, and, importantly, significant drops in the partial pressure of oxygen (PO₂). Information from these chemoreceptors is relayed to the brainstem respiratory centers to adjust ventilation accordingly. For instance, an increase in PCO₂ (hypercapnia) or a decrease in pH (acidosis) will stimulate increased breathing to expel more CO₂ and restore normal levels. Stretch receptors in the lungs (Hering-Breuer reflex), irritant receptors in the airways, and input from higher brain centers (e.g., cerebral cortex for voluntary control, limbic system for emotional influences) also modulate breathing patterns.
Adaptations to High-Altitude/Low-Oxygen Environments
When individuals ascend to high altitudes, they encounter an environment where the partial pressure of oxygen (PO₂) in the air is significantly lower, even though the percentage of oxygen (21%) remains the same. This condition, known as hypoxia, poses a physiological challenge to the respiratory and cardiovascular systems. The body has several mechanisms to adapt, both acutely (short-term) and chronically (long-term), to these low-oxygen conditions. Acutely, one of the first responses is an increase in ventilation (breathing rate and depth), a reaction triggered by peripheral chemoreceptors sensing the reduced arterial PO₂. This hyperventilation helps to increase alveolar PO₂, thereby improving oxygen uptake, but it also leads to increased CO₂ exhalation, which can cause respiratory alkalosis (an increase in blood pH).
Other acute adaptations include an increase in heart rate and cardiac output to improve oxygen delivery to tissues. Over a period of days to weeks, further acclimatization occurs. The kidneys respond to respiratory alkalosis by increasing the excretion of bicarbonate ions, which helps to normalize blood pH and allows ventilation to remain elevated. The body also starts to produce more red blood cells (polycythemia), triggered by the hormone erythropoietin released from the kidneys in response to hypoxia. More red blood cells mean a higher hemoglobin concentration and thus an increased oxygen-carrying capacity of the blood. Additionally, changes occur at the tissue level, such as an increase in the density of capillaries in muscles and an increase in the concentration of myoglobin (an oxygen-binding protein in muscle cells), both of which facilitate oxygen delivery and utilization.
Populations that have lived at high altitudes for many generations, such as Tibetans, Andeans, and Ethiopian highlanders, often exhibit distinct genetic adaptations that allow them to thrive in hypoxic environments. These adaptations can differ between populations. For example, Tibetans tend to maintain higher resting ventilation and have a blunted polycythemic response compared to acclimatized lowlanders, possibly avoiding the negative consequences of excessively thick blood. They also exhibit modifications in hemoglobin's affinity for oxygen and more efficient oxygen utilization at the cellular level. Studying these adaptations provides valuable insights into human physiological plasticity and the genetic basis of adaptation to environmental extremes.
Common Respiratory System Disorders
Despite its resilience, the respiratory system is susceptible to a wide range of disorders, from common infections to chronic conditions. Understanding these illnesses, their underlying mechanisms, diagnostic approaches, and the market for treatments is crucial for healthcare professionals and anyone interested in respiratory health.
Asthma and COPD Pathophysiology
Asthma and Chronic Obstructive Pulmonary Disease (COPD) are two of the most prevalent chronic respiratory diseases globally, yet they have distinct underlying pathophysiological mechanisms. Asthma is characterized by chronic inflammation of the airways, leading to reversible bronchoconstriction (narrowing of the airways), airway hyperresponsiveness (an exaggerated bronchoconstrictor response to various stimuli), and airway remodeling over time. This inflammation is often triggered by allergens (like pollen, dust mites, pet dander), irritants (smoke, pollution), respiratory infections, exercise, or even emotional stress. During an asthma attack, the smooth muscles surrounding the airways contract, the airway lining swells due to inflammation, and there is increased mucus production, all of which obstruct airflow and cause symptoms like wheezing, shortness of breath, chest tightness, and coughing.
COPD, on the other hand, is a progressive disease characterized by persistent airflow limitation that is not fully reversible. It typically encompasses two main conditions: chronic bronchitis and emphysema, though most individuals with COPD have features of both. Chronic bronchitis is defined by a chronic productive cough due to inflammation and excessive mucus production in the bronchi. Emphysema involves the destruction of the alveoli, the tiny air sacs where gas exchange occurs. This destruction leads to a loss of lung elasticity and a reduction in the surface area available for gas exchange, making it difficult to breathe, particularly during exhalation, leading to air trapping in the lungs. The primary cause of COPD is long-term exposure to irritants, most commonly cigarette smoke, but also air pollution, occupational dusts, and chemicals.
While both conditions involve airway inflammation and airflow obstruction, the nature of the inflammation and the structural changes differ. In asthma, the inflammation is predominantly eosinophilic and is generally responsive to corticosteroid treatment. In COPD, the inflammation is often neutrophilic and less responsive to corticosteroids. Furthermore, the airflow limitation in asthma is typically reversible, either spontaneously or with treatment, whereas in COPD, it is largely irreversible and progressive. Both diseases significantly impact quality of life and can have substantial economic consequences. For instance, in the United States, the annual direct and indirect costs associated with COPD and asthma run into billions of dollars.
This course provides a good starting point for understanding medical terminology related to various body systems, including respiratory disorders.
Pandemic-Related Conditions (e.g., COVID-19 Lung Impacts)
The COVID-19 pandemic, caused by the SARS-CoV-2 virus, brought respiratory illnesses to the forefront of global health concerns and highlighted the profound impact viruses can have on the lungs. While SARS-CoV-2 can affect multiple organ systems, the respiratory system is often the primary site of infection and severe disease. The virus typically enters the body through the respiratory tract and can infect cells lining the airways and alveoli. In many individuals, this leads to symptoms ranging from mild, cold-like illness to severe viral pneumonia.
In severe cases of COVID-19, the infection can trigger an excessive inflammatory response in the lungs, leading to widespread damage to the alveoli and surrounding blood vessels. This can result in Acute Respiratory Distress Syndrome (ARDS), a life-threatening condition characterized by severe hypoxia (low blood oxygen levels) and stiff, fluid-filled lungs. Patients with ARDS often require mechanical ventilation and intensive care. The inflammatory process can also lead to blood clots in the lungs (pulmonary embolism) and other complications. The damage caused by severe COVID-19 can be long-lasting, with some individuals experiencing persistent respiratory symptoms, reduced lung function, and abnormalities on lung imaging for months or even years after the initial infection – a condition often referred to as "Long COVID" or Post-Acute Sequelae of SARS-CoV-2 infection (PASC).
The pandemic spurred unprecedented research into viral pathogenesis, immune responses to respiratory infections, and the development of vaccines and antiviral therapies. It also underscored the importance of public health measures in controlling the spread of respiratory pathogens and the need for robust healthcare systems capable of managing surges in critically ill patients. Understanding the lung impacts of pandemic-related conditions like COVID-19 continues to be an active area of research, aiming to improve treatments for acute illness and manage the long-term consequences for survivors.
These courses offer a broad understanding of human physiology and how the body responds to diseases, which is relevant to understanding conditions like COVID-19.
Diagnostic Tools (Spirometry, Imaging)
Diagnosing respiratory disorders involves a combination of clinical assessment, patient history, and various diagnostic tools designed to evaluate lung function and visualize lung structures. Spirometry is one of the most common and fundamental pulmonary function tests (PFTs). It measures the amount (volume) and/or speed (flow) of air that can be inhaled and exhaled. During a spirometry test, the patient breathes into a mouthpiece connected to a spirometer. Key measurements include Forced Vital Capacity (FVC), the total amount of air exhaled forcefully after a maximal inhalation, and Forced Expiratory Volume in one second (FEV1), the amount of air exhaled in the first second of a forced expiration. The ratio of FEV1 to FVC (FEV1/FVC) is a crucial indicator of airflow obstruction, commonly seen in conditions like asthma and COPD.
Imaging techniques play a vital role in visualizing the structures of the chest and identifying abnormalities. Chest X-rays are often the first imaging test performed for respiratory symptoms, providing a general overview of the lungs, heart, and surrounding structures. They can help detect conditions like pneumonia, lung cancer, collapsed lung (pneumothorax), or fluid accumulation (pleural effusion). Computed Tomography (CT) scans of the chest provide much more detailed cross-sectional images of the lungs and can detect smaller or more subtle abnormalities that may not be visible on an X-ray. High-resolution CT (HRCT) is particularly useful for evaluating interstitial lung diseases and emphysema. Other imaging modalities like Magnetic Resonance Imaging (MRI) are less commonly used for primary lung assessment but can be valuable in specific situations, such as evaluating chest wall masses or cardiovascular structures related to the lungs.
Beyond spirometry and imaging, other diagnostic tools include pulse oximetry (a non-invasive method to measure blood oxygen saturation), arterial blood gas (ABG) analysis (which measures the levels of oxygen, carbon dioxide, and pH in arterial blood), bronchoscopy (a procedure where a thin, flexible tube with a camera is inserted into the airways to visualize them and obtain tissue samples), and various specialized PFTs to assess lung volumes, diffusion capacity, and airway responsiveness. The choice of diagnostic tools depends on the suspected condition and the clinical context, aiming for an accurate diagnosis to guide appropriate treatment.
Market Trends in Respiratory Pharmaceuticals
The market for respiratory pharmaceuticals is substantial and continues to grow, driven by several factors including the high prevalence of respiratory diseases like asthma, COPD, allergic rhinitis, and emerging threats such as respiratory infections. Globally, the respiratory drugs market was valued in the tens of billions of dollars annually and is projected to see continued growth with compound annual growth rates (CAGRs) generally in the range of 5-7% over the coming years. This growth is fueled by an aging global population (which is more susceptible to respiratory illnesses), increasing pollution levels, lifestyle changes, and ongoing advancements in drug development and delivery technologies.
Key therapeutic areas within the respiratory pharmaceutical market include treatments for asthma and COPD, which represent a significant portion of market revenue. Bronchodilators (such as beta-agonists and anticholinergics) and inhaled corticosteroids are mainstays of treatment. Combination therapies, which include both a long-acting bronchodilator and an inhaled corticosteroid in a single inhaler, have become increasingly common and are a major driver of market growth. Biologics (monoclonal antibodies) targeting specific inflammatory pathways have also emerged as important treatments for severe asthma and, more recently, for certain phenotypes of COPD, representing a high-growth segment within the market due to their targeted action and efficacy in difficult-to-treat patients.
Innovations in drug delivery systems, such as the development of smart inhalers that can track usage and provide feedback to patients and healthcare providers, are also shaping the market. There's also a growing interest in treatments for rarer respiratory conditions like idiopathic pulmonary fibrosis and cystic fibrosis, with significant research and development efforts focused on these areas. The Asia-Pacific region is expected to be a significant growth area for respiratory pharmaceuticals due to rising disease prevalence, improving healthcare infrastructure, and increasing healthcare expenditure. However, the market also faces challenges, including patent expirations of blockbuster drugs leading to generic competition, stringent regulatory requirements for new drug approvals, and pricing pressures from payers. Despite these challenges, the ongoing need for effective respiratory treatments ensures that this pharmaceutical sector will remain a critical and dynamic area of healthcare.
Career Pathways in Respiratory Health
A passion for understanding the respiratory system can lead to a variety of fulfilling career paths, each contributing to respiratory health in unique ways. From direct patient care to cutting-edge research and the development of life-saving medical devices, opportunities abound for those dedicated to helping people breathe easier. This section explores some prominent roles, industry positions, research avenues, and the certifications that can pave the way.
For those considering a career pivot or just starting, the field of respiratory health offers both challenges and immense rewards. It requires dedication, continuous learning, and a genuine desire to make a difference in people's lives. While the journey may seem daunting, remember that every expert was once a beginner. With perseverance and the right educational foundation, you can achieve your goals. The satisfaction of helping someone take a full, comfortable breath is a powerful motivator, and the diverse roles within this field mean there's likely a path that aligns with your unique skills and interests.
Pulmonology vs. Respiratory Therapy Roles
Two of the most recognized clinical roles in respiratory health are Pulmonologists and Respiratory Therapists (RTs). While both professionals are dedicated to patients with breathing problems, their training, scope of practice, and daily responsibilities differ significantly. A pulmonologist is a medical doctor (MD or DO) who has completed medical school, a residency in internal medicine, and then a fellowship specializing in pulmonary diseases. They diagnose and treat a wide range of complex respiratory conditions, including asthma, COPD, lung cancer, interstitial lung diseases, pulmonary hypertension, sleep disorders, and critical illnesses affecting the lungs. Pulmonologists can prescribe medications, order and interpret diagnostic tests, perform procedures like bronchoscopy, and manage patients in both outpatient clinics and hospital settings, including intensive care units (ICUs).
Respiratory Therapists, on the other hand, are allied health professionals who typically hold an associate's or bachelor's degree in respiratory therapy. They work under the direction of physicians, including pulmonologists, to evaluate, treat, and care for patients with breathing disorders. RTs are skilled in managing life support equipment such as mechanical ventilators, administering oxygen therapy, delivering aerosolized medications, performing pulmonary function tests, drawing arterial blood gases, and providing patient education on managing their respiratory conditions. They play a crucial role in emergency response for patients in respiratory distress and are integral members of the healthcare team in hospitals, ICUs, emergency rooms, neonatal units, long-term care facilities, and home care settings. The U.S. Bureau of Labor Statistics projects that employment of respiratory therapists is expected to grow 13 percent from 2023 to 2033, much faster than the average for all occupations, with about 8,200 openings projected each year. The median annual wage for respiratory therapists was $80,450 in May 2024. For physicians, including pulmonologists, overall employment is projected to grow 3 percent from 2022 to 2032. The demand for pulmonologists is also expected to rise due to an aging population and increasing prevalence of respiratory conditions, with some projections indicating a potential deficit of pulmonologists in the coming years.
Choosing between these paths depends on individual career goals, the desired level of autonomy, and the length of educational commitment. Pulmonology involves a longer and more intensive educational journey leading to a broader diagnostic and prescriptive authority. Respiratory therapy offers a more direct route into patient care with a strong focus on hands-on therapeutic interventions and equipment management. Both professions are vital and offer rewarding opportunities to impact patient lives positively.
This book is an essential resource for those interested in the practice of respiratory care, covering a wide range of topics relevant to respiratory therapists and pulmonologists.
Industry Roles in Medical Device Development
Beyond direct patient care, there are significant career opportunities in the medical device industry, particularly in the development, manufacturing, and marketing of respiratory care devices. The respiratory devices market is a multi-billion dollar global industry, with consistent growth driven by the rising prevalence of respiratory diseases, an aging population, and technological advancements. For example, the therapeutic respiratory devices market size was estimated at USD 12.5 billion in 2023 and is expected to grow at a CAGR of 5.8% from 2024 to 2030. Some analyses project even higher growth rates for the broader respiratory care devices market.
Professionals in this sector can hold various roles. Engineers (biomedical, mechanical, electrical, software) are crucial for designing and developing new devices, from complex ventilators and oxygen concentrators to portable nebulizers and smart inhalers. Regulatory affairs specialists navigate the complex approval processes required by bodies like the FDA in the U.S. or equivalent agencies in other countries, ensuring devices meet safety and efficacy standards. Clinical research associates and managers design and oversee clinical trials to test new devices. Sales and marketing professionals work to bring these products to hospitals, clinics, and home care providers. Quality assurance and manufacturing roles ensure that devices are produced to high standards.
Individuals with a clinical background, such as respiratory therapists or nurses with respiratory experience, are also highly valued in the industry. They can contribute as clinical specialists, providing training and support to users of the devices, or by offering insights into product design based on real-world clinical needs. The field is dynamic, with ongoing innovation focused on creating more effective, user-friendly, portable, and connected devices. This includes the integration of AI and data analytics for improved patient monitoring and personalized treatment. A career in the respiratory medical device industry offers the chance to contribute to technological advancements that directly improve patient care and quality of life.
For a foundational understanding of respiratory anatomy and physiology, which is crucial for device development, this book is a valuable resource.
Research Positions in Aerosol Drug Delivery
Research in aerosol drug delivery is a specialized and vital area within respiratory science, focusing on the development and optimization of methods to deliver medications directly to the lungs. This route of administration is preferred for many respiratory diseases like asthma and COPD because it allows drugs to act directly at the site of disease, potentially increasing efficacy and reducing systemic side effects. Research positions in this field can be found in academic institutions, pharmaceutical companies, and specialized research organizations.
Scientists in this area work on various aspects of aerosol drug delivery. This includes formulation science, where researchers develop drug formulations that are suitable for aerosolization and maintain stability and activity. It also involves device engineering, focusing on the design and performance of inhalers (like metered-dose inhalers, dry powder inhalers, and nebulizers) to ensure efficient and consistent drug delivery to the desired regions of the lung. Understanding aerosol physics – how particles are generated, their size distribution, transport, and deposition in the complex geometry of the airways – is fundamental to this research. Researchers use computational modeling, in vitro (laboratory-based) experiments, and in vivo (animal or human) studies to evaluate and improve drug delivery systems.
Key goals in aerosol drug delivery research include improving the efficiency of drug deposition in the lungs, enhancing patient adherence through easier-to-use devices, developing "smart" inhalers with feedback mechanisms, and exploring novel drug carriers like nanoparticles for targeted delivery. There is also significant interest in delivering not just small molecule drugs but also biologics (like proteins and nucleic acids) via the pulmonary route. A career in this research area requires a strong background in disciplines such as pharmaceutical sciences, biomedical engineering, chemical engineering, physics, or physiology, often with advanced degrees (Master's or PhD). It offers the opportunity to be at the forefront of innovation in respiratory medicine.
Entry-Level Certifications (e.g., CRT, RRT)
For individuals aspiring to become respiratory therapists, obtaining professional certification is a critical step and often a requirement for state licensure and employment. In the United States, the primary credentialing body for respiratory therapists is the National Board for Respiratory Care (NBRC). The NBRC offers two main entry-level credentials: the Certified Respiratory Therapist (CRT) and the Registered Respiratory Therapist (RRT).
To become a CRT, candidates must typically graduate from a respiratory therapy education program accredited by the Commission on Accreditation for Respiratory Care (CoARC). These programs are usually at the associate's degree level. After graduation, candidates must pass the Therapist Multiple-Choice (TMC) Examination administered by the NBRC. The CRT credential demonstrates competency in entry-level respiratory care practices and is often the minimum requirement for licensure in states that regulate the profession.
The RRT credential represents a higher level of expertise and is generally preferred by employers, often leading to more advanced roles and potentially higher salaries. To earn the RRT, candidates must also graduate from a CoARC-accredited respiratory therapy program (which can be an associate's or bachelor's degree program). They must pass the TMC Examination at a higher cut score than required for the CRT, and additionally, they must pass the Clinical Simulation Examination (CSE). The CSE is designed to evaluate a therapist's decision-making and problem-solving skills in various clinical scenarios. Many respiratory therapists pursue the RRT credential to enhance their career opportunities and demonstrate a higher level of proficiency. Beyond these primary credentials, the NBRC also offers specialty certifications for RRTs (and sometimes CRTs) in areas like neonatal/pediatric respiratory care (NPS), adult critical care (ACCS), and sleep disorders specialist (SDS), allowing therapists to further specialize their expertise.
Formal Education Requirements
Embarking on a career related to the respiratory system typically involves a structured educational path. Depending on the chosen profession, this can range from associate degrees to extensive medical training and specialized research doctorates. Understanding these requirements is the first step for anyone aspiring to work in this fascinating and vital field.
Undergraduate Prerequisites (Biology, Chemistry)
For most career paths in respiratory health, a strong foundation in the sciences at the undergraduate level is essential. Core prerequisite courses typically include general biology, general chemistry, and often organic chemistry and physics. These courses provide the fundamental knowledge of biological processes, chemical reactions, and physical principles that underpin human physiology and medical science. For instance, biology courses cover cellular structure and function, genetics, and organ systems, which are directly applicable to understanding the respiratory system. Chemistry is crucial for comprehending gas laws, acid-base balance, pharmacology, and the biochemical reactions involved in respiration and metabolism.
Beyond these core sciences, other beneficial undergraduate courses might include anatomy, physiology, microbiology, biochemistry, and statistics. Anatomy and physiology courses offer a detailed understanding of the structure and function of the human body, including an in-depth look at the respiratory system itself. Microbiology is important for understanding respiratory infections, while biochemistry delves into the molecular mechanisms of life. Statistics is increasingly vital for understanding research literature, participating in research, and for evidence-based practice in healthcare.
These prerequisites are not just hurdles to clear; they are the building blocks upon which more specialized knowledge is constructed. For students aiming for medical school (to become a pulmonologist), a bachelor's degree with a strong science GPA and successful completion of the Medical College Admission Test (MCAT) are standard requirements. For allied health programs like respiratory therapy, an associate's or bachelor's degree in respiratory care will have its own specific science prerequisites integrated into or required before starting the core curriculum. Aspiring researchers will also need a solid science background, often leading to a bachelor's degree in a relevant science field before pursuing graduate studies.
These courses offer a solid foundation in the biological sciences relevant to respiratory studies.
For a more specialized focus on anatomy and physiology related to respiratory care, consider this book:
Medical School vs. Allied Health Programs
The educational pathways to becoming a pulmonologist versus an allied health professional like a respiratory therapist are quite different in terms of length, intensity, and scope of training. Aspiring pulmonologists must first complete a bachelor's degree, typically with a strong emphasis on pre-medical science courses. This is followed by four years of medical school, where they gain a broad education in all aspects of medicine, including anatomy, physiology, pharmacology, pathology, and clinical skills. After medical school, they must complete a residency in internal medicine, which typically lasts three years. During residency, they receive supervised training in diagnosing and managing a wide range of adult medical conditions. Finally, to specialize in pulmonology, they undertake a fellowship in pulmonary disease, which usually takes an additional two to three years. Some may pursue further subspecialization in areas like critical care medicine or sleep medicine, adding more time to their training.
Allied health programs, such as those for respiratory therapists, offer a more direct route to a career in respiratory care. Respiratory therapy programs are available at the associate's degree level (typically two years) and the bachelor's degree level (typically four years). These programs are specifically focused on respiratory care and include coursework in anatomy, physiology, pharmacology, cardiopulmonary diagnostics, mechanical ventilation, and patient assessment, along with extensive clinical rotations in various healthcare settings. Upon graduation, individuals must pass national certification exams (CRT and RRT) to become credentialed and typically need to obtain state licensure to practice. While the educational commitment is shorter than for medical school, the curriculum is rigorous and specialized.
Other allied health professions related to respiratory health might include pulmonary function technologists, who specialize in performing a wide array of diagnostic lung function tests, or polysomnographic technologists, who work in sleep labs diagnosing sleep-related breathing disorders. The choice between medical school and an allied health program depends on an individual's career aspirations, interest in the depth and breadth of medical knowledge versus specialized technical skills, and the desired level of autonomy and responsibility in patient care. OpenCourser provides a vast library to explore courses in Health & Medicine to help you understand these pathways better.
This course provides a foundational understanding of human physiology, which is relevant for both medical and allied health pathways.
For those interested in a medical terminology foundation, which is useful across all healthcare roles:
Specialized Graduate Research Areas
For those inclined towards discovery and innovation in respiratory science, pursuing specialized graduate research offers a path to contribute to the fundamental understanding and treatment of respiratory diseases. A Master's or, more commonly, a Doctoral (PhD) degree is typically required for independent research careers. These programs are usually housed within university departments such as physiology, pharmacology, biomedical engineering, molecular biology, immunology, or public health, often with a focus on pulmonary science or a related discipline.
Specialized graduate research areas in respiratory science are diverse and continually evolving. Some researchers focus on the cellular and molecular mechanisms of lung diseases like asthma, COPD, cystic fibrosis, or idiopathic pulmonary fibrosis. This might involve studying gene expression, protein interactions, inflammatory pathways, or stem cell biology in the context of lung injury and repair. Others specialize in pulmonary immunology, investigating how the immune system protects the lungs from infection and how its dysregulation contributes to disease. Research into respiratory infections, including virology and bacteriology, is another critical area, particularly in the wake of pandemics.
Another significant area is aerosol science and drug delivery, focusing on developing more effective ways to deliver therapeutic agents to the lungs. Respiratory mechanics and physiology research explores the physical principles of breathing, gas exchange, and how these are altered in disease states. Some researchers delve into translational research, aiming to bridge the gap between basic science discoveries and clinical applications, such as developing new diagnostic tools or therapies. Epidemiological research investigates the patterns, causes, and effects of respiratory diseases in populations, including the impact of environmental factors like air pollution or occupational exposures. These specialized areas often overlap, encouraging interdisciplinary collaboration to tackle complex research questions.
While not graduate-level research courses, these options provide foundational knowledge that is essential before embarking on specialized research.
A comprehensive understanding of physiology, as offered in books like "Pulmonary Physiology," is crucial for any research in this field.
Accreditation Standards Across Countries
Accreditation plays a crucial role in ensuring the quality and consistency of education and training programs for healthcare professionals, including those in respiratory care and medicine. Accreditation standards and processes can vary significantly across countries, reflecting different healthcare systems, regulatory frameworks, and educational philosophies. However, the overarching goal is generally the same: to ensure that graduates possess the necessary knowledge, skills, and professional competencies to provide safe and effective patient care.
In the United States, for example, respiratory therapy education programs are accredited by the Commission on Accreditation for Respiratory Care (CoARC). CoARC sets standards for curriculum, faculty qualifications, resources, and student outcomes. Graduation from a CoARC-accredited program is a prerequisite for taking the NBRC certification exams (CRT and RRT), which are then used for state licensure. Medical schools in the U.S. are accredited by the Liaison Committee on Medical Education (LCME) or the American Osteopathic Association's Commission on Osteopathic College Accreditation (COCA). Residency and fellowship programs are accredited by the Accreditation Council for Graduate Medical Education (ACGME).
In other countries, different national or regional bodies oversee the accreditation of medical and allied health programs. For instance, in Canada, respiratory therapy programs are accredited by the Council on Accreditation for Respiratory Therapy Education (CoARTE). Medical schools and postgraduate training programs have their own accreditation bodies. European countries often follow standards outlined by frameworks like the European Union directives for professional qualifications, but specific accreditation processes are typically managed at the national level. International organizations, such as the World Federation for Medical Education (WFME), work to promote high standards in medical education globally and may recognize national accrediting agencies.
These accreditation standards are important for students as they ensure the quality of the education they receive and often impact their ability to become licensed or certified and practice in their chosen profession, both domestically and internationally. For individuals considering education or practice in a different country, it's essential to research the specific accreditation and licensure requirements of that jurisdiction. OpenCourser's extensive catalog can help you browse for courses from institutions around the world, allowing you to compare programs and understand different educational approaches.
Self-Directed Learning Strategies
Beyond formal education, the journey of understanding the respiratory system can be greatly enhanced by self-directed learning. This is particularly true for career-changers or independent learners who wish to deepen their knowledge or explore specific niches within respiratory science. Leveraging online resources, engaging with case studies, and undertaking projects can create a rich and flexible learning experience.
Online courses are exceptionally well-suited for building a foundational understanding or supplementing existing knowledge in complex topics like the respiratory system. They offer the flexibility to learn at one's own pace and often provide access to a wide range of materials, from video lectures by experts to interactive simulations. Professionals can use online courses to stay updated on the latest advancements in respiratory care, diagnostics, or treatment modalities, fulfilling continuing education requirements or simply enhancing their current practice. Students can utilize them to reinforce concepts learned in traditional classrooms or to explore areas not covered in their core curriculum. OpenCourser's Learner's Guide offers valuable tips on how to create a structured curriculum and make the most of online learning.
Simulation Tools for Respiratory Mechanics
Understanding the mechanics of breathing – how air moves in and out, how pressures change, and how lung volumes are affected – can be challenging from textbooks alone. Simulation tools, often available online or as software, offer an interactive way to visualize and experiment with these concepts. These tools can range from simple animations demonstrating diaphragmatic movement and lung expansion to more complex models that allow users to manipulate variables like airway resistance, lung compliance, or respiratory rate and observe the effects on airflow and pressure-volume loops.
For students, these simulations can bring abstract physiological principles to life. For example, a simulation might allow you to model an asthma attack by increasing airway resistance and observe the resulting difficulty in exhalation and changes in lung volumes. Similarly, you could simulate conditions like emphysema (with increased compliance) or pulmonary fibrosis (with decreased compliance) to see how these diseases affect the work of breathing. Some advanced simulations are used in medical training to practice managing patients on mechanical ventilators, allowing learners to adjust ventilator settings and see the physiological responses in a safe, virtual environment.
Engaging with these tools helps solidify understanding of concepts like Boyle's Law in action, the role of elastic recoil, and the interplay of different pressures (atmospheric, intra-alveolar, intrapleural). Many online courses incorporate such simulations, or you can find standalone resources. Actively using these tools, predicting outcomes before changing parameters, and then analyzing the results is a powerful self-directed learning strategy. OpenCourser features many courses that might incorporate such tools, and searching for "respiratory physiology simulations" or "virtual respiratory labs" on the platform could yield relevant learning opportunities.
These courses may introduce or discuss principles that are often demonstrated using simulation tools.
Case Study Analysis of Rare Disorders
Analyzing case studies, particularly those involving rare respiratory disorders, is an excellent method for deepening understanding and developing clinical reasoning skills. Rare diseases, while individually uncommon, collectively affect a significant number of people and often present unique diagnostic and management challenges. By studying these cases, learners can move beyond textbook descriptions to see how diseases manifest in real patients, how diagnostic processes unfold, and how treatment decisions are made in complex situations.
Many medical journals publish case reports, and online databases dedicated to rare diseases often feature detailed case descriptions. When analyzing a case study, it's beneficial to consider several aspects: What were the presenting symptoms and patient history? What diagnostic tests were performed, and why? How were the results interpreted? What was the differential diagnosis, and how was the final diagnosis reached? What were the treatment options, and what was the rationale for the chosen approach? What was the patient's outcome, and what are the long-term implications of the disorder?
This process encourages critical thinking and helps integrate knowledge from different areas, such as anatomy, physiology, pathology, and pharmacology. For example, a case study on alpha-1 antitrypsin deficiency could illuminate the genetic basis of a lung disease, its impact on alveolar structure (leading to emphysema), and the specific therapies available. Similarly, exploring cases of rare interstitial lung diseases or congenital respiratory anomalies can provide insights into less common pathophysiological mechanisms. For self-directed learners, discussing case studies with peers or mentors, if possible, can further enhance the learning experience by providing different perspectives and clarifying complex points.
While not directly case-study focused, understanding the fundamentals from courses like these is essential before tackling complex case analyses.
Books focusing on clinical aspects of respiratory medicine often use case studies as teaching tools. "Respiratory Care" is a comprehensive text that would support such learning.
Virtual Lab Experiences
For learners without access to physical laboratory facilities, virtual labs offer an invaluable alternative for gaining practical insights into respiratory physiology and diagnostics. These online platforms and software applications simulate experimental setups and procedures, allowing users to conduct experiments, collect data, and analyze results in a digital environment. Virtual labs can cover a wide range of topics relevant to the respiratory system, from basic physiological measurements to more complex diagnostic simulations.
For instance, a virtual lab might allow a student to perform a simulated spirometry test on a virtual patient, guiding them through the procedure, data collection, and interpretation of FEV1, FVC, and FEV1/FVC ratios. Another virtual experiment could involve manipulating gas concentrations and observing their effects on simulated breathing patterns or oxygen saturation. Some platforms offer histology simulations where users can examine virtual slides of lung tissue, identifying different cell types and pathological changes. More advanced virtual labs might even simulate aspects of research, such as drug testing on virtual cell cultures or modeling the effects of genetic mutations on lung function.
The benefits of virtual labs include accessibility, safety (no risk of handling hazardous materials or damaging expensive equipment), and the ability to repeat experiments easily. They can be particularly useful for reinforcing concepts learned in lectures or readings by providing a hands-on, albeit simulated, experience. Many online courses are now incorporating virtual lab components to enhance the learning experience. When engaging with virtual labs, it's important to actively participate, follow protocols carefully (even if simulated), and critically analyze the generated data, just as one would in a physical lab setting. OpenCourser's platform can be a great place to find courses from Science or Health & Medicine that might offer such virtual experiences.
Courses focused on physiology often cover principles demonstrated in lab settings, making virtual lab experiences highly complementary.
Capstone Project Ideas (e.g., Ventilator Design)
Engaging in a capstone project is a powerful way for self-directed learners or students in formal programs to consolidate their knowledge and apply it to a real-world problem or creative endeavor related to the respiratory system. A capstone project typically involves in-depth research, critical thinking, problem-solving, and often, the creation of a tangible output. For those interested in the intersection of engineering and respiratory care, a project focusing on aspects of ventilator design could be highly rewarding, though complex.
Simpler, yet still valuable, capstone project ideas could include developing an educational module on a specific respiratory disease for a lay audience, creating a detailed review of current research on a niche topic like the long-term respiratory effects of a particular environmental toxin, or designing a public health campaign to promote lung health in a specific community. One could also analyze existing datasets (e.g., public health data on asthma prevalence) to identify trends and propose interventions, or develop a software tool to help patients manage their chronic respiratory condition (e.g., an asthma action plan app). For those with programming skills, creating a simple simulation of a physiological process, like gas exchange or the mechanics of breathing, could be a feasible project.
The key to a successful capstone project is choosing a topic that is both interesting to the learner and manageable within their available resources and timeframe. It should allow for the application of knowledge gained through courses and self-study. Even if a project like "ventilator design" is too ambitious in its entirety for an individual, one could focus on a specific component, such as researching user interface improvements for existing ventilators, analyzing the fluid dynamics of a particular valve design, or developing an algorithm for a specific ventilation mode. Such projects not only deepen understanding but also develop valuable skills in research, project management, and communication, which are highly transferable to various career paths. When selecting a project, consider leveraging the resources available on platforms like OpenCourser to find relevant courses or books that can support your research and development efforts. Remember, a well-executed project can also serve as a significant portfolio piece when seeking employment or further educational opportunities.
This comprehensive book on mechanical ventilation could provide a wealth of information and inspiration for a capstone project related to ventilator design or application.
Emerging Technologies in Respiratory Care
The field of respiratory care is continually evolving, with technological advancements playing a pivotal role in improving diagnosis, treatment, and management of respiratory conditions. From artificial intelligence to regenerative medicine, innovative approaches are transforming how healthcare professionals address breathing disorders and enhance patient outcomes. Staying abreast of these emerging technologies is crucial for practitioners, researchers, and anyone involved in the future of respiratory health.
The pace of innovation is rapid, with significant investments driving the development of smarter, more personalized, and less invasive solutions. These technologies not only aim to improve clinical efficacy but also to enhance patient quality of life, increase accessibility to care, and optimize healthcare resources. For those entering the field, understanding these trends can highlight exciting areas for specialization and career development.
AI-Driven Diagnostic Systems
Artificial intelligence (AI) and machine learning (ML) are making significant inroads into respiratory diagnostics, offering the potential to enhance accuracy, speed up diagnoses, and identify subtle patterns that might be missed by human observers. AI algorithms are being developed to analyze various types of medical data, including imaging scans (like chest X-rays and CT scans), pulmonary function test results, breath sounds, and even patient-reported symptoms. For instance, AI systems can be trained to detect signs of pneumonia, lung nodules (potentially cancerous), or patterns indicative of interstitial lung diseases on chest images with a level of accuracy comparable to, or sometimes exceeding, that of radiologists.
Beyond image analysis, AI is being applied to the interpretation of spirometry data to better classify obstructive and restrictive lung diseases or predict disease progression. Machine learning models are also being used to analyze cough sounds or breath patterns recorded by smartphones or wearable sensors to screen for conditions like asthma, COPD, or respiratory infections. These technologies could enable earlier detection of exacerbations or the onset of disease, potentially leading to more timely interventions. Some AI systems are being developed to integrate data from multiple sources – imaging, PFTs, electronic health records, and genetic information – to provide more comprehensive diagnostic assessments and personalized risk predictions. While AI holds immense promise, challenges remain in terms of data quality, algorithm validation, regulatory approval, and integration into clinical workflows. Nevertheless, AI-driven diagnostic systems are poised to become increasingly important tools in the arsenal of respiratory healthcare.
The integration of AI with respiratory devices is also contributing to the growing efficacy and demand of therapeutic respiratory devices. For example, AI-supported wearable technology is showing promise in accurately diagnosing COPD and forecasting exacerbations. As technology continues to evolve, the field of Artificial Intelligence will undoubtedly play a larger role in medicine.
3D-Printed Tracheal Implants
Regenerative medicine and tissue engineering are offering new hopes for treating complex structural problems in the respiratory system, and 3D bioprinting is an emerging technology at the forefront of these efforts. For conditions involving severe damage or congenital defects of the trachea (windpipe) or large airways, reconstructive options have traditionally been limited and often associated with significant complications. 3D printing allows for the creation of custom-designed scaffolds that can precisely match a patient's anatomy. These scaffolds can be made from biocompatible materials that support cell growth and tissue regeneration.
Researchers are exploring various approaches to creating 3D-printed tracheal implants. Some involve printing a porous scaffold that can then be seeded with the patient's own cells (such as chondrocytes for cartilage formation and epithelial cells for lining the airway) in a bioreactor before implantation. The idea is that these cells will grow and differentiate on the scaffold, eventually forming a new, functional segment of the trachea. Other strategies focus on printing directly with bio-inks that contain cells and biomaterials, aiming to create a living tissue construct from the outset. The advantages of 3D-printed implants include the potential for personalized design, reduced risk of immune rejection if the patient's own cells are used, and the ability to create complex structures that mimic natural tissue.
While this technology is still largely in the experimental and early clinical trial stages, it holds significant promise for patients with conditions like tracheal stenosis (narrowing), tracheomalacia (weakness of tracheal walls), or extensive tracheal damage from trauma or cancer. Challenges that researchers are working to overcome include ensuring adequate vascularization (blood supply) of the implant, achieving proper mechanical strength and flexibility, preventing infection, and long-term integration and function of the engineered tissue. As 3D printing technology and our understanding of tissue regeneration continue to advance, custom-made airway implants could become a viable treatment option in the future.
Portable Oxygen Concentrators
For individuals with chronic respiratory conditions like COPD, cystic fibrosis, or severe asthma who require long-term oxygen therapy (LTOT), portable oxygen concentrators (POCs) have revolutionized their ability to maintain mobility and quality of life. Traditionally, patients needing oxygen outside the home relied on heavy compressed oxygen tanks or liquid oxygen systems, which can be cumbersome and have limited supply. POCs, in contrast, are medical devices that extract oxygen from the ambient air, concentrate it, and deliver it to the patient, offering a continuous and potentially unlimited supply as long as there is power (either from a battery or an electrical outlet).
POCs work by drawing in room air (which is about 21% oxygen and 78% nitrogen) and passing it through a series of molecular sieves (often made of zeolite) that selectively adsorb nitrogen, allowing concentrated oxygen (typically 87-96%) to pass through and be delivered to the patient via a nasal cannula. Most POCs are designed to be lightweight and compact, some weighing as little as a few pounds, and can be carried in a shoulder bag or pulled on a small cart. They offer various flow settings, including continuous flow (delivering oxygen at a constant rate) and pulse dose (delivering a bolus of oxygen only when the patient inhales), which helps conserve battery life.
The development of smaller, lighter, and more efficient POCs with longer battery life is an ongoing trend in the respiratory device market. These advancements have significantly improved the independence of patients requiring oxygen, allowing them to travel, work, and participate more fully in daily activities. However, it's crucial that patients use POCs as prescribed by their healthcare provider, as the appropriate device and flow settings depend on individual oxygen needs, which can vary at rest, during activity, and during sleep. The market for POCs is expected to continue growing due to the increasing prevalence of chronic respiratory diseases and the growing demand for home-based and patient-centric care solutions.
The course "Vital Signs: Understanding What the Body Is Telling Us" can provide context on why oxygen therapy is crucial for some patients.
This book provides comprehensive information on respiratory care practices, including oxygen therapy.
Gene Therapy for Cystic Fibrosis
Cystic Fibrosis (CF) is a genetic disorder caused by mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene. This gene provides instructions for making a protein that functions as a channel for the movement of chloride ions across cell membranes. Defective CFTR protein leads to thick, sticky mucus accumulation, particularly in the lungs and digestive system, resulting in chronic lung infections, progressive lung damage, and other complications. Gene therapy aims to correct the underlying genetic defect by delivering a functional copy of the CFTR gene to the affected cells in the lungs.
The concept of gene therapy for CF has been pursued for decades, but it has faced significant challenges. One major hurdle is efficiently and safely delivering the therapeutic gene to a sufficient number of target cells in the airways (primarily the airway epithelial cells) to achieve a clinical benefit. Various viral vectors (modified viruses that can carry genetic material into cells, such as adenoviruses, adeno-associated viruses, and lentiviruses) and non-viral methods (like lipid nanoparticles) have been investigated as delivery vehicles. Another challenge is ensuring long-term expression of the functional CFTR gene, as airway epithelial cells are constantly turning over. The immune response to viral vectors can also limit the effectiveness of repeated treatments.
Despite these obstacles, research continues, and newer gene editing technologies like CRISPR-Cas9 are also being explored for their potential to directly correct the CFTR gene mutations in a patient's own cells. While CFTR modulator therapies (small molecule drugs that help improve the function of the defective CFTR protein in patients with specific mutations) have dramatically improved outcomes for many people with CF, they are not a cure and are not effective for all mutations. Gene therapy holds the promise of a more definitive treatment that could benefit a broader range of individuals with CF by addressing the root cause of the disease. Clinical trials are ongoing, and while a widely available gene therapy for CF is not yet a reality, the field is advancing, driven by a deeper understanding of gene delivery mechanisms and molecular biology.
Ethical Challenges in Respiratory Medicine
The practice of respiratory medicine, like all medical fields, is fraught with complex ethical challenges. These dilemmas often arise at the intersection of limited resources, patient autonomy, public health imperatives, and social justice concerns. Navigating these issues requires careful consideration, open dialogue, and a commitment to ethical principles.
Ventilator Allocation During Shortages
One of the most acute ethical challenges in respiratory medicine, starkly highlighted during the COVID-19 pandemic, is the allocation of scarce life-saving resources like mechanical ventilators during public health emergencies or mass casualty events. When the demand for ventilators outstrips supply, healthcare providers and institutions face the agonizing task of deciding which patients receive this critical support and which do not. Such decisions involve profound moral considerations and have life-or-death consequences.
Various ethical frameworks and guidelines have been proposed to assist in these difficult situations. These often attempt to balance principles such as saving the most lives, prioritizing those with the best chance of survival, ensuring fairness and equity, and respecting patient autonomy. Some allocation protocols incorporate clinical criteria, such as prognosis or likelihood of short-term survival, while others might consider factors like age or instrumental value (e.g., prioritizing healthcare workers). However, many of these criteria are contentious and raise concerns about discrimination, particularly against older adults or individuals with disabilities or pre-existing conditions.
The development of fair, transparent, and ethically sound ventilator allocation policies is crucial. This process should ideally involve input from clinicians, ethicists, legal experts, and the public. Clear communication with patients and families is also paramount during such crises. The challenge underscores the need for robust public health preparedness, including strategies to surge critical care capacity and stockpile essential medical supplies, to minimize the likelihood of having to make such tragic choices. Moreover, it emphasizes the importance of ongoing societal discussions about resource allocation in healthcare, even outside of crisis situations.
This comprehensive text on mechanical ventilation touches upon many aspects of its use, and the ethical considerations are an inherent part of critical care practice.
Smoking Cessation Policy Dilemmas
Tobacco smoking is the leading preventable cause of respiratory diseases, including lung cancer, COPD, and exacerbations of asthma. Therefore, policies aimed at promoting smoking cessation and preventing smoking initiation are critical public health interventions. However, these policies often give rise to ethical dilemmas, balancing public health goals with individual liberties, economic interests, and concerns about fairness.
One set of dilemmas revolves around the extent to which governments should intervene to discourage smoking. Measures like increased taxation on tobacco products, comprehensive bans on advertising and promotion, graphic warning labels, and restrictions on smoking in public places have proven effective in reducing smoking rates. Ethically, these are often justified by the principles of beneficence (promoting health) and non-maleficence (preventing harm), particularly given the harm smoking causes to non-smokers through secondhand smoke. However, some argue that such policies infringe on individual autonomy and the right to make personal lifestyle choices, even if those choices are unhealthy. There are also concerns about the regressive nature of tobacco taxes, which disproportionately affect low-income individuals who are also more likely to smoke.
Another area of ethical debate concerns access to and funding for smoking cessation services. While effective treatments exist (including counseling, nicotine replacement therapy, and other medications), access can be limited, especially for underserved populations. Questions arise about whether healthcare systems and insurers have an ethical obligation to provide comprehensive and affordable cessation support. Furthermore, the rise of e-cigarettes and other novel nicotine products has introduced new policy dilemmas, with debates about their potential role in harm reduction versus concerns about youth initiation and long-term health effects. Navigating these dilemmas requires careful consideration of scientific evidence, ethical principles, and the potential for unintended consequences, aiming for policies that are both effective in improving public health and respectful of individual rights.
Clinical Trial Disparities in Low-Income Countries
Clinical trials are essential for advancing medical knowledge and developing new treatments for respiratory diseases. However, significant disparities exist in where these trials are conducted and who participates in them, with low- and middle-income countries (LMICs) often being underrepresented. This underrepresentation can have profound ethical and practical consequences. Many respiratory diseases, such as tuberculosis and pneumonia, disproportionately affect populations in LMICs, yet treatments are often developed and tested primarily in high-income countries (HICs).
Conducting clinical trials in LMICs presents unique ethical challenges. There are concerns about potential exploitation, where populations with limited access to healthcare might be enrolled in trials without fully understanding the risks and benefits, or without assurance of access to the treatment if it proves effective (the principle of post-trial access). Ensuring truly informed consent can be difficult due to language barriers, lower literacy rates, and cultural differences. Moreover, the research infrastructure, including ethics review boards and regulatory oversight, may be less developed in some LMICs, raising concerns about participant protection and data quality. An analysis of patent trends and clinical trials related to respiratory tract infections in Asia highlighted that industry often has less interest in developing diagnostics, which are crucial in LMICs, compared to therapeutics, and that most diagnostic studies were financed by universities and hospitals rather than industry.
Addressing these disparities is an ethical imperative. It requires building research capacity in LMICs, fostering equitable partnerships between researchers from HICs and LMICs, and ensuring that research agendas are relevant to the health needs of the host communities. Ethical review processes must be robust and culturally sensitive. Furthermore, there should be a commitment to benefit-sharing, ensuring that communities participating in research gain tangible benefits, such as improved healthcare infrastructure or access to effective treatments. Promoting greater inclusion of diverse populations in clinical trials globally is not only a matter of justice but also essential for ensuring that medical advancements are safe and effective for everyone who might need them.
Environmental Justice in Air Quality Management
Environmental justice refers to the fair treatment and meaningful involvement of all people regardless of race, color, national origin, or income, with respect to the development, implementation, and enforcement of environmental laws, regulations, and policies. In the context of respiratory health, environmental justice is a critical concern because exposure to air pollution is often inequitably distributed, with low-income communities and communities of color disproportionately burdened by higher levels of pollutants and their associated health impacts.
These disparities arise from a variety of factors, including the historical siting of polluting industries, major roadways, and waste disposal facilities in or near marginalized communities. These communities may also have less political power to resist such developments or advocate for cleaner air. The consequences are severe, leading to higher rates of asthma, COPD, and other respiratory illnesses, as well as increased hospitalizations and premature deaths in these overburdened neighborhoods. The World Health Organization has noted that people in low- and middle-income countries disproportionately experience the burden of outdoor air pollution.
Addressing environmental injustice in air quality management requires a multi-pronged approach. This includes strengthening air quality monitoring in vulnerable communities, implementing stricter emissions standards for industrial facilities, promoting cleaner transportation options, and investing in green infrastructure. It also involves ensuring that affected communities have a meaningful voice in decision-making processes related to environmental permits and land use planning. Policies should be designed to reduce pollution in the most affected areas and prevent the creation of new pollution hotspots. From an ethical standpoint, achieving environmental justice in air quality is about upholding the right to a healthy environment for all and addressing systemic inequities that contribute to health disparities. This intersects with broader social justice movements and requires a commitment from policymakers, public health officials, and community advocates.
Frequently Asked Questions
Navigating the world of respiratory health, whether for academic, career, or personal interest, often brings up many questions. This section aims to address some common inquiries, particularly those relevant to career transitions and the evolving landscape of respiratory care.
Can respiratory therapists become pulmonologists?
Yes, a respiratory therapist (RT) can become a pulmonologist, but it requires a significant additional educational and training commitment. The pathways are distinct. A respiratory therapist typically completes an associate's or bachelor's degree in respiratory therapy and then obtains certification and licensure. To become a pulmonologist, an individual must complete a bachelor's degree (fulfilling pre-medical requirements), attend four years of medical school to earn an MD or DO degree, complete a three-year residency in internal medicine, and then undertake a two-to-three-year fellowship specifically in pulmonary medicine. Some may pursue further fellowship training in critical care or sleep medicine.
Therefore, if an RT decides to become a pulmonologist, they would essentially need to start the medical education pathway from the undergraduate pre-medical preparation stage, apply to and complete medical school, and then follow the subsequent residency and fellowship training. While their prior experience as an RT would undoubtedly provide valuable clinical insights, a deep understanding of patient care in respiratory settings, and a strong foundation in respiratory physiology and equipment, it does not typically shorten the formal medical training required to become a physician specialist.
The decision to make such a transition involves weighing the extensive time, financial investment, and academic rigor of medical training against the desire for the expanded scope of practice, diagnostic responsibilities, and leadership roles associated with being a pulmonologist. Many RTs find fulfilling and advanced careers within respiratory therapy itself, progressing into roles in management, education, research, or specialized clinical practice areas like neonatal care or critical care, often with advanced degrees or certifications within the RT field. However, for those with the aspiration and dedication to pursue medicine, the background of an RT can be a strong asset.
How does automation threaten respiratory care jobs?
The impact of automation on respiratory care jobs is a nuanced topic. While some tasks may become more automated, it's unlikely that automation will wholly replace the need for skilled respiratory therapists or pulmonologists in the foreseeable future. Instead, automation is more likely to transform roles, augment capabilities, and potentially shift the focus of human practitioners towards more complex, patient-centered, and decision-making tasks.
For instance, AI-driven diagnostic tools might assist in interpreting imaging scans or pulmonary function tests, potentially speeding up workflows and improving accuracy. Robotic systems could be used for tasks like medication delivery or patient transport in some settings. Smart ventilators and monitoring systems can automate certain adjustments based on patient data, providing real-time feedback and alerts. However, these technologies typically require human oversight, interpretation, and intervention, especially in complex or unstable patients. The critical thinking, clinical judgment, communication skills, and empathetic patient interaction provided by human healthcare professionals are difficult to automate.
Instead of a direct threat, automation could free up respiratory care professionals from some routine or repetitive tasks, allowing them to focus on more complex patient assessments, personalized treatment planning, patient education, and interprofessional collaboration. It might also create new roles related to managing and interpreting data from these automated systems or developing and implementing new technologies. However, as with any field undergoing technological change, there will be a need for continuous learning and adaptation to new tools and workflows. The emphasis will likely shift towards skills that complement automation, such as advanced clinical reasoning, data analysis, and the human aspects of care that machines cannot replicate.
What global regions have respiratory specialist shortages?
Shortages of respiratory specialists, including pulmonologists and trained respiratory therapists, are a significant concern in many parts of the world, though the severity and nature of these shortages vary by region. Generally, low- and middle-income countries (LMICs) face the most acute shortages. These regions often have a high burden of respiratory diseases (like tuberculosis, pneumonia, and COPD exacerbated by indoor and outdoor air pollution) but limited healthcare infrastructure, fewer training programs for specialists, and challenges in retaining trained professionals due to "brain drain" to higher-income countries.
Even within high-income countries, disparities exist. Rural and underserved urban areas often have fewer specialists compared to affluent urban centers. For example, while the U.S. has a relatively high number of respiratory therapists per capita compared to many nations, access can be uneven. Projections in the U.S. have also indicated a potential future deficit of pulmonologists, partly due to an aging physician workforce and increasing demand from an aging population with more chronic respiratory conditions. In Europe, while many countries have well-developed healthcare systems, there can still be regional variations in the availability of specialized respiratory care, and the specific role and prevalence of "respiratory therapists" as a distinct profession can differ from the North American model.
Addressing these global shortages requires a multifaceted approach, including investing in training programs within underserved regions, developing strategies to retain healthcare workers, leveraging telehealth to extend the reach of specialists, and task-shifting certain responsibilities to other appropriately trained healthcare providers where feasible. International collaborations and support for strengthening healthcare systems in LMICs are also crucial. The World Health Organization often highlights the broader issue of health workforce shortages as a barrier to achieving universal health coverage.
Is hands-on training replaceable with virtual simulations?
Virtual simulations are increasingly valuable tools in healthcare education, including for respiratory care, but they are generally seen as a supplement to, rather than a complete replacement for, traditional hands-on training. Simulations can offer safe, repeatable, and accessible environments to practice skills, learn procedures, and develop clinical decision-making abilities. For example, students can practice ventilator management on a virtual patient, interpret simulated PFT results, or respond to various emergency scenarios without any risk to actual patients.
However, hands-on training provides experiences that are difficult to replicate fully in a virtual environment. These include the tactile feel of performing procedures, the nuances of patient communication and interaction, the ability to adapt to unexpected real-world variations, and the experience of working within a multidisciplinary team in a clinical setting. Developing fine motor skills, learning to manage equipment in real-time, and building the confidence that comes from direct patient care under supervision are crucial components of clinical competency that are best honed through hands-on practice.
The most effective educational models often blend both approaches. Virtual simulations can be used to build foundational knowledge and practice skills in a controlled setting, preparing students for real-world clinical experiences. This can make hands-on training more efficient and effective, as students arrive with a better understanding and baseline skill set. For continuing education and maintaining competency, simulations also offer a convenient way for practicing clinicians to refresh skills or learn new techniques. While technology will continue to enhance simulation capabilities, the human element and the complexities of real-world patient care ensure that hands-on training will remain an indispensable part of educating respiratory health professionals.
How volatile is respiratory device market investment?
Investment in the respiratory device market is generally considered to be relatively stable with strong growth potential, though like any market, it can be subject to certain volatilities and shifts. The underlying drivers for this market are robust: an aging global population, the high and often increasing prevalence of chronic respiratory diseases like asthma and COPD, the ongoing threat of respiratory infections (as highlighted by pandemics), and continuous technological advancements. These factors create a sustained demand for respiratory devices, from diagnostic tools to therapeutic equipment like ventilators, inhalers, and oxygen concentrators. For instance, various market reports project compound annual growth rates (CAGRs) for the respiratory devices market in the range of 5% to over 8% in the coming years, indicating a healthy investment landscape.
However, certain factors can introduce volatility. Regulatory changes and approval processes for new devices can be lengthy and uncertain, impacting timelines and return on investment. Healthcare reimbursement policies and budget constraints in healthcare systems can affect purchasing decisions for capital-intensive equipment. Competition within the market is also significant, with established players and new entrants vying for market share. Economic downturns can influence healthcare spending, although the essential nature of many respiratory devices often provides some insulation. Patent expirations for key technologies can also lead to increased competition from generic or similar devices.
Areas of particular investor interest currently include "smart" devices with connectivity and data analytics capabilities, portable and home-care-focused devices, and technologies incorporating AI. The COVID-19 pandemic, for example, led to a surge in demand and investment for ventilators and personal protective equipment, though this was an exceptional event. Overall, while specific segments or companies might experience fluctuations, the long-term outlook for investment in the respiratory device market remains positive due to fundamental demographic and health trends. Stakeholders interested in this market often consult detailed market analysis reports from firms like Grand View Research or Mordor Intelligence for specific forecasts and trends.
Do climate change policies affect respiratory careers?
Yes, climate change policies can, and likely will, increasingly affect respiratory careers, primarily by influencing the prevalence and nature of respiratory illnesses and by shaping public health priorities. Climate change contributes to worsening air quality through factors like increased frequency and intensity of wildfires (releasing smoke and particulate matter), higher ground-level ozone formation (due to warmer temperatures), and altered patterns of allergens like pollen. These environmental changes can exacerbate existing respiratory conditions such as asthma and COPD and may contribute to the development of new cases.
Policies aimed at mitigating climate change, such as transitioning to cleaner energy sources, improving energy efficiency, and promoting sustainable transportation, can have significant co-benefits for respiratory health by reducing air pollution. This could, over the long term, potentially reduce the burden of some pollution-related respiratory diseases. However, the health impacts of climate change already underway, and those projected for the future, will likely increase the demand for respiratory health services. For example, increased heatwaves can worsen respiratory conditions, and changes in infectious disease patterns (some of which may be respiratory) could also be influenced by climate shifts.
For respiratory health professionals, this means an evolving landscape. There may be an increased need for expertise in managing conditions exacerbated by environmental factors, a greater role in public health advocacy for policies that protect air quality and address climate change, and opportunities to participate in research on the links between climate, air quality, and respiratory health. Careers in environmental health, public health policy, and research related to climate change's impact on health will also likely see growth. Therefore, while climate mitigation policies aim to improve health outcomes, the ongoing effects of climate change will ensure a continued, and possibly intensified, need for skilled respiratory care professionals who are knowledgeable about these broader environmental determinants of health.
Useful Links and Resources
To further your exploration of the respiratory system and related careers, here are some valuable online resources:
The American Lung Association: A leading organization dedicated to lung health, offering extensive information on respiratory diseases, advocacy, and research. You can visit their website at www.lung.org.
The National Heart, Lung, and Blood Institute (NHLBI): Part of the U.S. National Institutes of Health, the NHLBI conducts and supports research related to heart, lung, and blood diseases. Their website, www.nhlbi.nih.gov, is a rich source of information for both professionals and the public.
The World Health Organization (WHO) - Respiratory Diseases: Provides global perspectives on respiratory health, including statistics, fact sheets on various conditions, and information on global strategies to combat respiratory diseases. Explore their resources at WHO Chronic Respiratory Diseases.
The National Board for Respiratory Care (NBRC): The credentialing body for respiratory therapists in the U.S. Their website, www.nbrc.org, provides information on certifications and the profession.
OpenCourser: For finding courses related to biology, medicine, and specific aspects of the respiratory system, OpenCourser's browse page is an excellent starting point. You can also check out the deals section for potential savings on relevant online courses.
Embarking on a journey to understand the respiratory system, whether for academic enrichment, career development, or personal health knowledge, is a rewarding endeavor. This intricate system, essential for life itself, offers endless avenues for discovery and impact. We hope this guide has provided a comprehensive overview and the necessary encouragement to explore this fascinating field further. With dedication and the wealth of resources available, including those on OpenCourser, you are well-equipped to continue learning and potentially contribute to the world of respiratory health.