Clinical Pharmacist
Clinical Pharmacist: A Comprehensive Career Guide
Clinical pharmacists are vital members of the healthcare team who specialize in the science of medications and their use in patient care. They work directly with physicians, other health professionals, and patients to ensure that prescribed medications achieve the best possible health outcomes. This involves not just dispensing drugs, but actively managing medication therapy, monitoring patient progress, and providing expert advice on drug selection, dosing, and potential side effects.
If you are drawn to a career that combines deep scientific knowledge with direct patient interaction and collaborative problem-solving within a healthcare setting, clinical pharmacy offers a compelling path. Imagine optimizing a complex medication regimen for a patient with multiple chronic conditions, preventing a harmful drug interaction, or educating a patient to manage their medications safely at home. These are the kinds of impactful contributions clinical pharmacists make daily.
Introduction to Clinical Pharmacist Careers
Understanding the role of a clinical pharmacist begins with recognizing their specialized focus within the broader field of pharmacy. They apply their in-depth knowledge of pharmacotherapy—the treatment of disease through medication—to provide direct patient care.
What is Clinical Pharmacy?
Clinical pharmacy is a health science discipline where pharmacists provide patient care that optimizes medication therapy and promotes health, wellness, and disease prevention. Unlike traditional pharmacy roles that might focus primarily on dispensing medications, clinical pharmacists are integral members of the healthcare team, often working in hospitals, clinics, or physician offices.
Their responsibilities extend beyond simply filling prescriptions. They assess patients' health status, evaluate the appropriateness and effectiveness of medications, and identify untreated health problems that could benefit from medication therapy. They collaborate closely with physicians and other providers to develop and implement medication plans tailored to each patient's specific needs and goals.
The scope involves direct patient interaction, medication therapy management (MTM), counseling, and monitoring patient outcomes. Clinical pharmacists use their expertise to ensure medications are used safely and effectively, contributing significantly to patient care and overall health system performance.
The Evolution of the Clinical Pharmacist Role
The role of the pharmacist has evolved significantly over the decades. Historically viewed primarily as dispensers of medication, pharmacists began moving towards a more patient-centered model in the latter half of the 20th century. This shift was driven by the increasing complexity of drug therapies and a growing recognition of the need for medication experts within clinical teams.
The development of Doctor of Pharmacy (PharmD) programs as the entry-level degree further solidified this transition, emphasizing clinical training and patient care skills. Today, clinical pharmacists are recognized as indispensable providers who improve medication use quality and safety.
Their integration into general practice teams and specialized clinics continues to grow. This expansion reflects a broader trend in healthcare towards team-based care, where the specialized knowledge of clinical pharmacists is leveraged to manage complex medication needs, particularly for patients with chronic conditions or those taking multiple medications (polypharmacy).
Distinguishing Clinical Pharmacists
It's important to differentiate clinical pharmacists from other pharmacy roles, particularly retail or community pharmacists. While both are highly trained medication experts, their primary focus and work environments differ significantly. Retail pharmacists typically work in community settings like chain or independent pharmacies, focusing on dispensing medications accurately, counseling patients on usage, and managing pharmacy operations.
Clinical pharmacists, conversely, work primarily in direct patient care settings such as hospitals, clinics, physicians' offices, or long-term care facilities. Their role is deeply integrated into the clinical team, involving collaboration with doctors and nurses to manage patient medication regimens, monitor for adverse effects, adjust dosages, and make therapeutic recommendations. They often have less focus on the dispensing process and more on optimizing therapy outcomes.
Furthermore, many clinical pharmacists pursue postgraduate residency training (PGY1 and/or PGY2) and board certification in specialized areas (like cardiology, oncology, or critical care), reflecting a depth of clinical expertise often required for their roles. While some retail pharmacists also engage in clinical services like vaccinations or MTM, the depth and scope of direct patient care are hallmarks of the clinical pharmacist role.
Common Work Settings
Clinical pharmacists practice in a diverse range of healthcare environments where they interact regularly with patients and other healthcare professionals. Hospitals are a major employment setting, where they work on general medicine floors, intensive care units, emergency departments, or specialized units like oncology or cardiology.
Ambulatory care clinics are another common setting. Here, clinical pharmacists manage chronic diseases (like diabetes, hypertension, anticoagulation), provide MTM services, and educate patients in an outpatient environment, often working alongside physicians in primary care or specialty clinics.
Other settings include long-term care facilities, home healthcare services, managed care organizations, government agencies (like the Veterans Affairs system), and academic institutions where they combine clinical practice with teaching and research. The specific environment often dictates the focus of their practice, but the core remains optimizing medication therapy through direct patient involvement.
Roles and Responsibilities of a Clinical Pharmacist
The daily work of a clinical pharmacist revolves around ensuring medications contribute positively to patient health. This involves a blend of direct patient care, collaboration, and specialized knowledge application.
Direct Patient Care and Medication Management
A core function of clinical pharmacists is direct patient interaction to manage medication therapy. This often involves conducting comprehensive medication reviews, where they assess all of a patient's medications (prescription, over-the-counter, supplements) to identify potential problems like drug interactions, inappropriate dosing, or therapeutic duplication.
They counsel patients on how to take their medications correctly, what side effects to expect, and the importance of adherence. This patient education is crucial for empowering individuals to manage their health effectively. Clinical pharmacists often take responsibility for managing patients with chronic conditions, adjusting therapies based on clinical guidelines and patient response.
Activities like developing personalized care plans, setting therapeutic goals, and monitoring progress are central to their patient care duties. Their expertise ensures that medication regimens are not just prescribed, but actively managed for optimal outcomes.
Collaboration within Healthcare Teams
Clinical pharmacists rarely work in isolation. They are integral members of multidisciplinary healthcare teams, collaborating closely with physicians, nurses, physician assistants, and other providers. This teamwork ensures coordinated and comprehensive patient care.
They provide expert consultations to physicians regarding drug selection, dosing adjustments, and managing adverse effects. During patient rounds in hospitals or team meetings in clinics, they contribute medication-related insights that inform overall treatment strategies. This collaborative approach helps prevent medication errors and optimizes therapeutic plans.
Their ability to communicate effectively with diverse team members and advocate for evidence-based medication use is essential. They serve as the primary medication resource for the team, bridging the gap between prescribing decisions and safe medication administration.
Drug Therapy Optimization
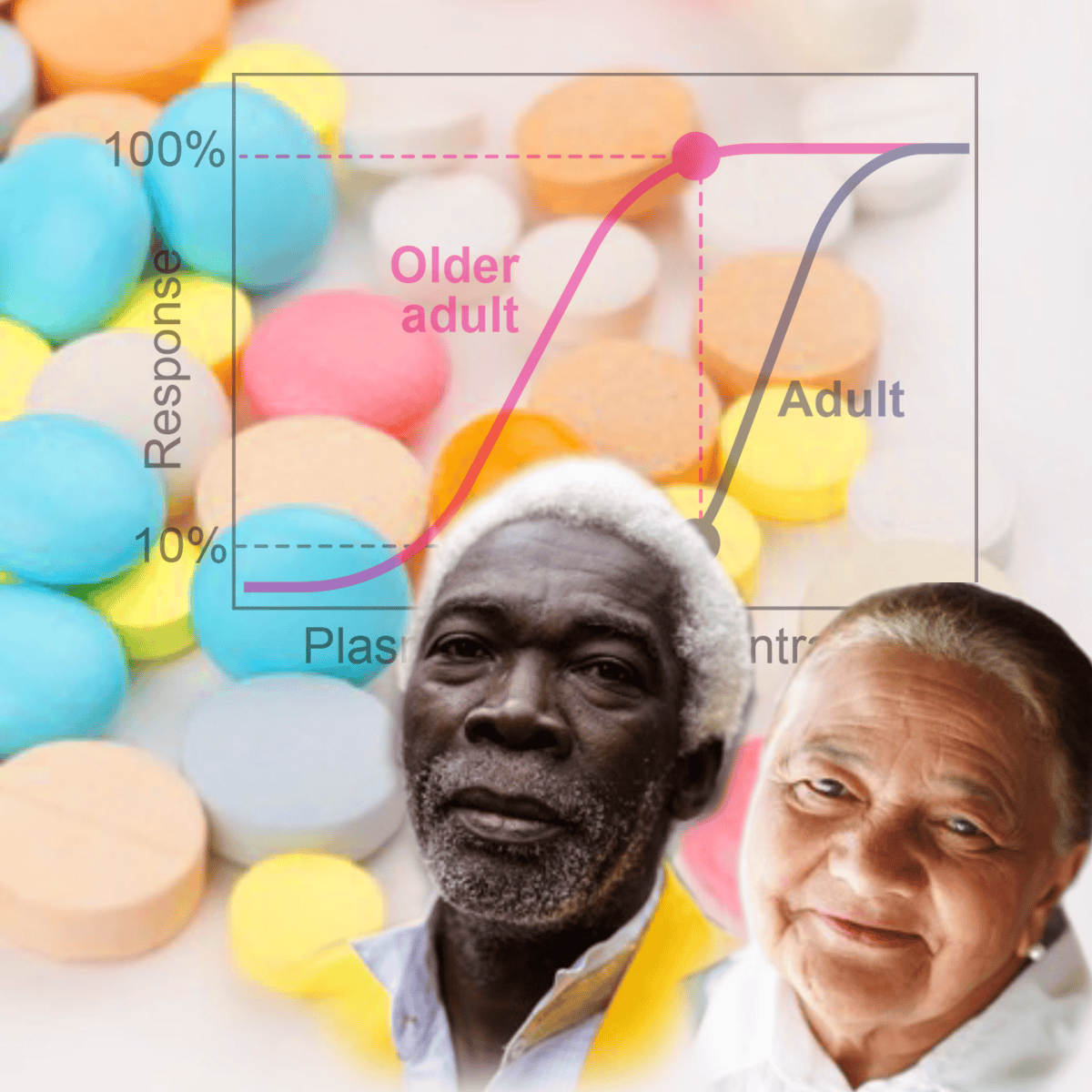
Optimizing drug therapy involves ensuring that medications are appropriate, effective, safe, and convenient for the patient. Clinical pharmacists use their deep understanding of pharmacology, pharmacokinetics (how the body processes drugs), and therapeutics to achieve this.
They evaluate prescribed medications against patient-specific factors like age, kidney and liver function, other medical conditions, and concurrent medications. They monitor patients for therapeutic effects and adverse drug reactions, recommending adjustments as needed. This may involve suggesting alternative medications, changing dosages, or discontinuing unnecessary drugs.
Tools like therapeutic drug monitoring (TDM) are often employed for medications with narrow therapeutic windows, ensuring drug levels remain within a safe and effective range. Their goal is always to maximize benefit and minimize harm from medications.
These foundational texts offer comprehensive knowledge in pharmacology, essential for drug therapy optimization.
Specialized Clinical Roles
Many clinical pharmacists pursue specialization in specific areas of practice, requiring advanced training, often through PGY2 residencies and board certification. These specialists develop profound expertise in managing complex patient populations or disease states.
Examples include oncology pharmacists who manage complex chemotherapy regimens, infectious diseases pharmacists involved in antimicrobial stewardship programs to combat antibiotic resistance, critical care pharmacists managing medications in the ICU, or ambulatory care pharmacists focusing on chronic disease management in outpatient settings.
Other specializations exist in areas like pediatrics, geriatrics, psychiatry, cardiology, solid organ transplantation, and nutrition support. These specialized roles allow clinical pharmacists to provide highly targeted, expert-level care within their chosen field, often serving as leaders and key resources within their institutions.
These courses provide focused knowledge relevant to specialized clinical roles, such as antimicrobial stewardship and geriatric pharmacotherapy.
Formal Education Pathways to Become a Clinical Pharmacist
Becoming a clinical pharmacist involves a rigorous and structured educational path, typically culminating in a doctoral degree followed by postgraduate training.
Foundational Undergraduate Studies
The journey begins with undergraduate coursework focused heavily on the sciences. Aspiring pharmacists typically complete two to four years of pre-pharmacy studies at a college or university before applying to a PharmD program. While some programs accept students after two years, many applicants hold a bachelor's degree.
Core prerequisite courses usually include general chemistry, organic chemistry, biology, physics, and mathematics (calculus). Strong performance in these foundational science courses is crucial for success in the demanding PharmD curriculum. Courses in anatomy, physiology, microbiology, and biochemistry are also highly recommended or required.
Beyond academics, experiences like volunteering or working as a pharmacy technician can strengthen an application by demonstrating commitment to the field and familiarity with pharmacy practice.
The Doctor of Pharmacy (PharmD) Program
The Doctor of Pharmacy (PharmD) is the required degree to become a licensed pharmacist in the United States. PharmD programs are typically four years in length (following pre-pharmacy studies) and are accredited by the Accreditation Council for Pharmacy Education (ACPE).
The curriculum combines didactic coursework in pharmaceutical sciences (pharmacology, medicinal chemistry, pharmaceutics) and clinical sciences (pharmacotherapy, patient assessment) with extensive experiential learning. The final year is usually dedicated entirely to advanced pharmacy practice experiences (APPEs), or rotations, in various settings like hospitals, clinics, and community pharmacies.
These rotations provide hands-on experience in direct patient care, medication management, and interprofessional collaboration, preparing graduates for practice. Admission to PharmD programs is competitive, requiring strong academics, prerequisite completion, often the Pharmacy College Admission Test (PCAT), letters of recommendation, and an interview.
Postgraduate Training: Residencies and Fellowships
While not always mandatory for licensure, postgraduate residency training is increasingly becoming the standard, especially for clinical pharmacists seeking hospital or specialized roles. Postgraduate Year One (PGY1) residencies offer generalized clinical training across various practice areas over 12 months.
Postgraduate Year Two (PGY2) residencies provide specialized training in a specific area, such as critical care, oncology, infectious diseases, or ambulatory care. Completing a PGY2 residency is often necessary for highly specialized clinical positions and academic roles.
Pharmacy residencies are competitive, utilizing a matching process similar to medical residencies, managed by the American Society of Health-System Pharmacists (ASHP). Fellowships are another postgraduate option, typically focused on research training rather than clinical practice.
According to ASHP Match data, residency positions have grown, but competition remains significant. In the 2024 Phase I Match, 4,916 individuals matched with programs, but 956 positions remained for Phase II, indicating a gap between applicants and available slots, though match rates remain relatively high for those participating.
Board Certification and Specialization
After completing residency training or gaining sufficient practice experience, clinical pharmacists can pursue board certification to demonstrate advanced expertise in a specialty area. The Board of Pharmacy Specialties (BPS) is the primary organization offering certification.
BPS currently recognizes numerous specialties, including Pharmacotherapy (BCPS), Ambulatory Care Pharmacy (BCACP), Cardiology Pharmacy (BCCP), Critical Care Pharmacy (BCCCP), Infectious Diseases Pharmacy (BCIDP), Oncology Pharmacy (BCOP), Pediatric Pharmacy (BCPPS), and Psychiatric Pharmacy (BCPP).
Eligibility typically requires graduation from an accredited PharmD program, current licensure, completion of relevant postgraduate training (usually a PGY2 residency in the specialty) or a set amount of practice experience (often 3-4 years), and passing a rigorous certification examination. Board certification signifies a high level of competence and often enhances career opportunities and earning potential.
Developing Skills Through Online Learning and Self-Study
While formal education provides the necessary foundation, continuous learning is crucial in pharmacy. Online courses and self-study can supplement formal training, help prepare for exams, and allow exploration of specialized areas.
Building Foundational Knowledge Online
Online learning platforms offer valuable resources for reinforcing core pharmacy concepts. Courses covering pharmacology, pharmacotherapy principles, and pathophysiology can help students solidify their understanding or allow practitioners to refresh their knowledge.
These resources can be particularly useful for those preparing for pharmacy school, supplementing challenging coursework, or even for individuals considering a career pivot who want to gauge their aptitude for the subject matter before committing to a full degree program.
Exploring courses on platforms like OpenCourser allows learners to find materials ranging from introductory concepts to more advanced topics, often taught by university faculty or industry experts. This flexible learning format can fit around existing commitments.
These courses offer foundational knowledge in pharmacology and drug information, suitable for building a strong base.
These books provide essential background in microbiology and medicinal chemistry, complementing online learning.
Preparing for Licensure and Certification
Online resources can be instrumental in preparing for the North American Pharmacist Licensure Examination (NAPLEX) and the Multistate Pharmacy Jurisprudence Examination (MPJE), which are required for licensure in the US. Review courses, question banks, and practice exams are widely available online.
Similarly, pharmacists preparing for BPS board certification exams can find specialized online courses and study materials tailored to specific specialty areas. These resources help focus study efforts and identify knowledge gaps.
Utilizing online tools for exam preparation allows for self-paced learning and targeted review, complementing knowledge gained through formal education and practice experience.
This course focuses on pharmaceutical calculations, a critical skill tested in licensure exams and essential for practice.
Exploring Specialized Pharmacy Topics
Online courses provide an accessible way to delve into specialized areas of clinical pharmacy without committing to a full residency or fellowship immediately. Topics like oncology, infectious diseases, cardiology, or psychiatric pharmacy may have dedicated courses available online.
This allows pharmacists or students to explore areas of interest, gain introductory knowledge, and potentially decide on future specialization paths. It's also valuable for established pharmacists looking to expand their knowledge base into new therapeutic areas relevant to their patient population.
OpenCourser's catalog, searchable by topic, can help identify courses in specific clinical niches within Health & Medicine.
These texts delve into specialized areas like antimicrobials and biotechnology, relevant for further exploration.
Enhancing Learning with Self-Directed Projects
Supplementing online coursework with practical application enhances learning. Self-directed projects, such as analyzing published clinical case studies, researching and presenting on a specific drug therapy topic, or developing a hypothetical medication management plan for a complex patient profile, can deepen understanding.
Analyzing complex patient cases allows learners to apply pharmacotherapeutic principles in a simulated real-world scenario. This active learning approach helps bridge the gap between theoretical knowledge and practical application.
Engaging in such projects can also build critical thinking and problem-solving skills essential for a clinical pharmacist. Documenting these projects can be beneficial for residency applications or career development.
This course introduces translational science, bridging research discoveries and healthcare practices, relevant for those interested in applying evidence through projects.
Career Progression for Clinical Pharmacists
A career as a clinical pharmacist offers various pathways for growth, specialization, and leadership, moving beyond entry-level roles.
Starting Your Career in Clinical Pharmacy
Most graduates enter the field after completing their PharmD and obtaining licensure. Those without residency training might start in staff pharmacist roles in hospitals or potentially some entry-level clinical positions, often gaining experience in medication distribution and basic clinical services.
However, completing a PGY1 residency significantly broadens opportunities, making graduates competitive for general clinical pharmacist positions in hospitals or ambulatory care settings. These roles typically involve direct patient care activities, medication order review, and participation in interdisciplinary rounds.
Early-career pharmacists focus on building clinical skills, gaining experience across different patient populations, and understanding healthcare system processes. Mentorship from senior pharmacists is often a key component of this stage.
Advancing through Specialization
Mid-career progression often involves specialization. Completing a PGY2 residency in a specific area like critical care, cardiology, oncology, infectious diseases, or ambulatory care allows pharmacists to become clinical specialists.
Board certification in a chosen specialty further solidifies expertise and is often required or preferred for specialist positions. Clinical specialists take on more complex patient cases within their area, develop practice guidelines, lead quality improvement initiatives, and serve as expert resources for the healthcare team.
This specialization allows for deeper clinical impact and often leads to greater autonomy and recognition within the healthcare system. It's a common path for those passionate about a particular area of pharmacotherapy.
This handbook is a practical reference for pharmacotherapy, useful for pharmacists at all stages, including specialization.
Leadership and Management Opportunities
Experienced clinical pharmacists can move into leadership and management roles within pharmacy departments or healthcare systems. Positions like clinical coordinator, pharmacy supervisor, or pharmacy director involve overseeing clinical services, managing staff, developing budgets, and ensuring regulatory compliance.
These roles require strong leadership, communication, and organizational skills, in addition to clinical expertise. Some pharmacists pursue further education, like a Master of Health Administration (MHA) or Master of Business Administration (MBA), to prepare for management responsibilities.
Leadership pathways offer opportunities to influence pharmacy practice on a broader scale, implement system-wide improvements, and mentor junior pharmacists.
Academia and Research Paths
For those interested in teaching and research, careers in academia are an option. Clinical pharmacy practice faculty positions at colleges of pharmacy involve teaching PharmD students, precepting students and residents during clinical rotations, providing clinical services at an affiliated practice site, and conducting scholarly research.
These roles typically require completion of residency training (often both PGY1 and PGY2) and sometimes a research fellowship or PhD, especially for research-intensive positions. Academic careers allow pharmacists to shape the next generation of practitioners and contribute to the evidence base through research.
Clinical pharmacists may also work in clinical research settings, such as with pharmaceutical companies or contract research organizations, contributing to drug development and clinical trials.
Key Industry Trends Shaping Clinical Pharmacy
The field of clinical pharmacy is dynamic, influenced by broader shifts in healthcare delivery, technology, and policy.
The Rise of Telepharmacy
Telehealth and telepharmacy services have expanded significantly, accelerated by recent events but driven by underlying needs for greater access and convenience. Clinical pharmacists are increasingly using technology to provide remote consultations, medication management, and patient monitoring.
Telepharmacy allows pharmacists to reach patients in rural or underserved areas, improve medication adherence through virtual check-ins, and provide specialized consultations remotely. This trend increases the efficiency and reach of clinical pharmacy services.
As technology evolves and reimbursement models adapt, telepharmacy is expected to become an even more integrated part of routine practice, offering new ways for clinical pharmacists to engage with patients and collaborate with providers.
Impact of Value-Based Care
The healthcare system's shift from fee-for-service to value-based care models rewards providers for quality outcomes and cost-efficiency rather than volume of services. Clinical pharmacists play a crucial role in this paradigm by optimizing medication use, preventing adverse drug events, improving adherence, and managing chronic diseases effectively – all contributing to better patient outcomes and lower overall healthcare costs.
Their expertise in medication management directly aligns with the goals of value-based care, such as reducing hospital readmissions and improving quality metrics (e.g., HEDIS, Star ratings). This trend elevates the importance of clinical pharmacists within healthcare organizations striving to meet value-based targets.
Organizations are increasingly recognizing the return on investment provided by clinical pharmacy services in achieving better health outcomes efficiently. According to research from MGMA, telehealth enhances value-based care metrics by reducing costs and improving patient access and satisfaction.
Personalized Medicine and Biologics
Advances in genomics and biotechnology are leading to more personalized approaches to medicine. Pharmacogenomics, the study of how genes affect a person's response to drugs, allows for tailoring medication choices and dosages based on an individual's genetic makeup.
Clinical pharmacists with expertise in pharmacogenomics can help interpret genetic test results and guide therapy decisions. The increasing use of complex biologic therapies also requires specialized knowledge regarding their administration, monitoring, and management of potential side effects.
Clinical pharmacists are essential in navigating the complexities of these advanced therapies, ensuring patients receive the most effective and safe treatments based on their unique characteristics.
This text covers clinical chemistry and molecular diagnostics, areas increasingly relevant with the rise of personalized medicine.
Evolving Regulatory Landscape
State regulations governing pharmacy practice are continually evolving, particularly regarding pharmacists' scope of practice, including prescriptive authority. Many states are expanding pharmacists' ability to prescribe certain medications independently or under collaborative practice agreements (CPAs) with physicians.
This expansion allows pharmacists to initiate or adjust therapies for specific conditions (e.g., hormonal contraceptives, naloxone, tobacco cessation products, travel medications, minor ailments) or manage chronic diseases more autonomously. While prescriptive authority varies significantly by state, the trend reflects growing recognition of pharmacists' capabilities.
Clinical pharmacists must stay informed about the specific laws and regulations in their state of practice, as these directly impact their ability to provide care and collaborate effectively within the healthcare system. Data from sources like GoodRx Health highlights the state-by-state variations in pharmacist prescribing authority.
Tools and Technologies in Clinical Pharmacy Practice
Clinical pharmacists rely on various tools and technologies to effectively manage patient care and ensure medication safety.
Leveraging Electronic Health Records (EHRs)
Electronic Health Record (EHR) systems are fundamental tools in modern healthcare settings. Clinical pharmacists use EHRs extensively to review patient histories, medication lists, lab results, and physician notes. This comprehensive view is essential for making informed decisions about medication therapy.
EHRs often include clinical decision support (CDS) features, such as alerts for potential drug interactions, allergies, or inappropriate dosing, which aid pharmacists in identifying and preventing medication errors. Pharmacists also use EHRs to document their interventions, recommendations, and patient progress notes, ensuring clear communication within the healthcare team.
Proficiency in navigating and utilizing EHR systems effectively is a critical skill for clinical pharmacists, enabling efficient workflow and access to vital patient information.
Utilizing Therapeutic Drug Monitoring (TDM) Tools
For certain medications with a narrow therapeutic index (where the effective dose is close to the toxic dose), Therapeutic Drug Monitoring (TDM) is crucial. Clinical pharmacists use TDM principles and software tools to interpret drug concentration levels in a patient's blood.
Based on these levels, patient-specific factors, and clinical response, pharmacists recommend dosage adjustments to maintain concentrations within the desired therapeutic range, maximizing efficacy while minimizing toxicity. This requires a strong understanding of pharmacokinetics and pharmacodynamics.
Software programs can assist with pharmacokinetic calculations and modeling, helping pharmacists predict how dosage changes will affect drug levels. TDM is commonly applied to drugs like certain antibiotics (e.g., vancomycin, aminoglycosides), anticonvulsants, and immunosuppressants.
Mastering Medication Reconciliation
Medication reconciliation is a formal process aimed at creating the most accurate list possible of all medications a patient is taking — including drug name, dosage, frequency, and route — and comparing that list against physician orders, transfer records, or discharge instructions. The goal is to avoid errors like omissions, duplications, dosing errors, or drug interactions during transitions of care (e.g., hospital admission, transfer, discharge).
Clinical pharmacists often lead or play a key role in the medication reconciliation process due to their expertise in medications. They interview patients, review records, and communicate with providers to resolve any discrepancies identified.
Effective medication reconciliation is a critical patient safety strategy, and pharmacists utilize systematic approaches and sometimes specific software tools to perform this task thoroughly.
Applying Evidence-Based Practice Principles
Clinical pharmacy practice is grounded in evidence-based medicine (EBM). Pharmacists use their skills to critically evaluate medical literature, clinical guidelines, and drug information resources to make informed, evidence-based recommendations for patient care.
Tools include access to biomedical databases (like PubMed), drug information compendia (such as Lexicomp, Micromedex), and published clinical practice guidelines (e.g., from professional societies or organizations like NICE in the UK). Staying current with the latest research and guidelines is essential.
Applying EBM involves integrating the best available evidence with clinical expertise and patient-specific values and preferences to guide therapeutic decisions. This rigorous approach ensures that patient care is based on sound scientific footing.
These resources support evidence-based practice by providing access to guidelines and continuous learning opportunities.
Ethical Considerations in Clinical Pharmacy
Clinical pharmacists frequently encounter complex ethical situations that require careful judgment and adherence to professional principles.
Navigating Medication Access and Affordability
The high cost of medications presents significant ethical challenges. Clinical pharmacists often work with patients who struggle to afford necessary treatments. They may need to help find cost-effective alternatives, navigate insurance formularies, or connect patients with assistance programs.
Balancing the need for optimal therapy with the reality of patient financial constraints requires sensitivity and resourcefulness. Ethical dilemmas can arise when the most effective treatment is unaffordable, forcing difficult choices about therapeutic alternatives.
Advocating for patient access to affordable medications while adhering to evidence-based practice principles is a key ethical responsibility for clinical pharmacists.
Ethical Decisions in Complex Care Scenarios
Clinical pharmacists participate in care teams managing patients with complex or life-limiting conditions, including end-of-life care. Ethical considerations arise regarding decisions about initiating, withholding, or withdrawing medication therapy, particularly when patient preferences, surrogate decision-maker input, and clinical appropriateness may conflict.
Issues related to patient autonomy, beneficence (acting in the patient's best interest), non-maleficence (avoiding harm), and justice (fairness) are often at the forefront. Pharmacists contribute their expertise on the benefits and burdens of medication therapies to inform these difficult ethical discussions.
Maintaining patient confidentiality and respecting diverse cultural or religious beliefs that influence healthcare decisions are also critical ethical duties in these complex scenarios.
Addressing Off-Label Drug Use
Off-label drug use refers to prescribing a medication for a condition, dose, or patient population not specifically approved by regulatory agencies like the FDA. While common and sometimes necessary based on emerging evidence or lack of approved alternatives, it raises ethical considerations.
Clinical pharmacists must evaluate the evidence supporting off-label use, assess the potential risks and benefits for the individual patient, and ensure informed consent is obtained. They play a role in ensuring off-label prescribing is based on sound clinical rationale and not driven by inappropriate influences.
Transparency with patients about the off-label nature of a treatment and careful monitoring are essential when such therapies are employed.
Managing Conflicts of Interest
Clinical pharmacists may interact with the pharmaceutical industry through research collaborations, educational programs, or consulting arrangements. It is crucial to manage these relationships ethically to avoid potential or perceived conflicts of interest that could compromise patient care or objectivity.
Disclosure of financial relationships and adherence to institutional policies regarding industry interactions are important safeguards. Ethical practice demands that therapeutic decisions always prioritize the patient's best interests, free from undue commercial influence.
Maintaining professional integrity and transparency in all interactions, particularly those involving pharmaceutical companies, is paramount.
Global Perspectives on Clinical Pharmacy
The practice of clinical pharmacy varies across the globe, influenced by different healthcare systems, regulations, and educational standards.
International Variations in Practice Scope
The scope of practice for clinical pharmacists differs significantly from country to country. In some nations, like the US, UK, Canada, and Australia, clinical pharmacists have well-established roles within healthcare teams, often with advanced training requirements and sometimes prescriptive authority.
In other regions, the clinical pharmacy role may be less developed or primarily focused on hospital settings, with limited direct patient care responsibilities or autonomy. Educational pathways and regulatory frameworks also vary widely.
Understanding these international differences is important for pharmacists considering practice abroad or collaborating with international colleagues.
Credential Recognition Across Borders
Pharmacists trained in one country who wish to practice in another typically face challenges with credential recognition. Licensing requirements, educational equivalencies, and examinations vary substantially between nations.
Obtaining licensure in a foreign country often requires undergoing specific assessments, additional training, or examinations to meet local standards. Organizations like the National Association of Boards of Pharmacy (NABP) in the US provide processes for foreign pharmacy graduates seeking licensure, but it can be a complex and lengthy undertaking.
Researching the specific requirements of the destination country well in advance is crucial for pharmacists considering international practice.
Opportunities in Global Health
Clinical pharmacists can contribute significantly to global health initiatives, particularly in resource-limited settings. Their expertise in medication management, supply chain logistics, and public health can help address challenges like infectious disease control, access to essential medicines, and improving medication safety.
Opportunities may exist with non-governmental organizations (NGOs), government agencies, or international health bodies. These roles often require adaptability, cultural sensitivity, and skills beyond traditional clinical practice, such as program management or health systems strengthening.
Working in global health offers a chance to apply pharmacy skills to address pressing health disparities and make a difference on an international scale.
The Importance of Cultural Competency
Regardless of practice location, cultural competency is essential for clinical pharmacists. Patients come from diverse cultural backgrounds that influence their beliefs about health, illness, and medication use. Understanding and respecting these differences is crucial for effective communication and patient care.
Culturally competent pharmacists can tailor patient education, build trust, and address potential barriers to medication adherence related to cultural factors or health literacy levels. This involves self-awareness of one's own biases and a commitment to learning about the cultural contexts of the patient populations served.
Providing patient-centered care requires recognizing and responding effectively to the diverse cultural needs of individuals and communities.
Frequently Asked Questions about Clinical Pharmacy Careers
Here are answers to some common questions about pursuing a career as a clinical pharmacist.
How does clinical pharmacy differ from retail pharmacy?
Clinical pharmacists primarily work in healthcare settings like hospitals and clinics, focusing on optimizing medication therapy as part of a healthcare team. They have extensive direct patient care responsibilities, manage complex regimens, and often require postgraduate residency training. Retail (community) pharmacists work in store settings, focus heavily on dispensing medications accurately, provide patient counseling on medication use, and manage pharmacy operations. While both roles require a PharmD, the emphasis and daily activities differ significantly.
Can clinical pharmacists prescribe medications?
Prescribing authority for pharmacists varies greatly by state in the US. Many states allow pharmacists to prescribe certain medications under specific protocols (e.g., naloxone, birth control, immunizations) or through collaborative practice agreements (CPAs) with physicians. Some states, like New Mexico and North Carolina, have pathways for advanced practice pharmacists (pharmacist clinicians or clinical pharmacist practitioners) to gain broader prescriptive authority, sometimes including controlled substances, often requiring additional training and certification. It's essential to check the specific regulations in the state of practice.
What is the job growth outlook for this field?
The U.S. Bureau of Labor Statistics (BLS) projects overall employment for pharmacists to grow 5 percent from 2023 to 2033, about as fast as the average for all occupations. This translates to about 14,200 openings per year, mainly due to retirements and workforce transitions. However, growth is expected to be stronger in clinical settings like hospitals and clinics compared to traditional retail pharmacies, driven by the aging population, complexity of medications, and the shift towards team-based, value-based care models where clinical pharmacists play a key role.
How competitive are residency programs?
Pharmacy residency programs, particularly PGY1 and specialized PGY2 programs, are competitive. According to ASHP data, while the number of residency positions has grown, the number of applicants often exceeds the available slots. Match rates vary year to year, but securing a position, especially in desirable programs or specialties, requires a strong academic record, relevant experience (like internships or research), good letters of recommendation, and strong interview skills. Phase I match rates for participants are generally high (often around 80%+ for those who actively participate and rank programs), but a significant number of positions and applicants proceed to Phase II of the Match.
Do clinical pharmacists work directly with patients?
Yes, direct patient interaction is a cornerstone of clinical pharmacy. Clinical pharmacists assess patients, take medication histories, provide education and counseling on medications, monitor for effectiveness and side effects, develop care plans, and make therapy recommendations often in collaboration with patients and their families. The extent of direct interaction varies by role and setting but is generally much higher than in traditional dispensing-focused roles.
What metrics define success in this role?
Success for a clinical pharmacist is often measured by their impact on patient outcomes and medication safety. Key metrics might include improvements in clinical markers (e.g., blood pressure control, A1c levels for diabetes), reductions in medication errors or adverse drug events, improved patient adherence to therapy, cost savings achieved through optimized medication use (e.g., preventing costly hospitalizations), and positive feedback from patients and collaborating healthcare providers. Contributions to quality improvement initiatives and adherence to evidence-based guidelines are also important indicators.
Useful Resources
For those exploring a career in clinical pharmacy, several organizations and resources provide valuable information:
- American College of Clinical Pharmacy (ACCP): Offers resources on clinical pharmacy practice, education, and research.
- American Society of Health-System Pharmacists (ASHP): Provides information on residency programs, accreditation, and practice standards, particularly for hospital and health-system settings.
- Bureau of Labor Statistics (BLS) Occupational Outlook Handbook - Pharmacists: Offers data on job outlook, salary, and work environments.
- National Association of Boards of Pharmacy (NABP): Information on licensure exams (NAPLEX, MPJE) and state board requirements.
- Board of Pharmacy Specialties (BPS): Details on specialty certifications available to pharmacists.
- OpenCourser Health & Medicine Category: Explore online courses related to pharmacy, pharmacology, and healthcare to supplement your learning journey.
Embarking on a career as a clinical pharmacist requires dedication, rigorous training, and a passion for patient care and the science of medication. It is a challenging yet highly rewarding profession that plays an increasingly critical role in modern healthcare. We hope this guide provides a comprehensive overview to help you determine if this path aligns with your aspirations.