Registered Nurse
Registered Nurse: A Comprehensive Career Guide
Registered Nurses (RNs) are foundational pillars of the healthcare system. They provide direct patient care, administer treatments, educate patients and families, and support physicians and other healthcare providers. An RN's work blends scientific knowledge, technical skill, and compassionate care, making it a demanding yet profoundly rewarding profession.
Working as an RN offers diverse opportunities to make a tangible difference in people's lives. Whether assisting in critical surgeries, comforting a worried patient, managing chronic conditions, or contributing to public health initiatives, the impact is direct and meaningful. The field also provides numerous pathways for specialization and career growth, catering to a wide range of interests and aptitudes within the healthcare landscape.
Introduction to Registered Nursing
What is a Registered Nurse?
A Registered Nurse (RN) is a licensed healthcare professional trained to provide and coordinate patient care. Their responsibilities are broad, encompassing tasks like assessing patient health problems and needs, developing and implementing nursing care plans, and maintaining medical records. They administer medications and treatments, operate medical equipment, and perform diagnostic tests.
RNs also play a crucial role in patient education, teaching individuals and their families how to manage illnesses or injuries. They offer advice on health maintenance and disease prevention. Their work involves critical thinking, sound judgment, and the ability to collaborate effectively within a healthcare team.
Essentially, RNs act as patient advocates, ensuring individuals receive appropriate care while navigating the complexities of the healthcare system. They combine technical proficiency with empathy, addressing both the physical and emotional needs of those under their care.
A Brief History of Nursing
Nursing, as a practice of caring for the sick and vulnerable, has roots stretching back to antiquity. However, modern nursing as a formal profession largely began in the mid-19th century. Figures like Florence Nightingale established foundational principles during the Crimean War, emphasizing sanitation, evidence-based practice, and formal nurse education.
The late 19th and early 20th centuries saw the establishment of nursing schools and professional organizations, standardizing training and practice. Nursing roles expanded significantly during major global events like World Wars I and II, demanding more skilled nurses in various settings. This period solidified nursing as a respected and essential profession.
Technological advancements, increased understanding of diseases, and evolving healthcare systems continued to shape the profession throughout the 20th and into the 21st century. Nursing education became more formalized, moving towards university-based degree programs, and specialization became increasingly common.
For those interested in the broader historical context of medicine and its evolution, understanding its philosophical and scientific underpinnings can be enlightening. Exploring the history provides perspective on how current practices came to be.
The RN's Place in Modern Healthcare
In today's complex healthcare systems, RNs are indispensable. They work across a vast spectrum of settings, from hospitals and clinics to schools, homes, and community health centers. They form the largest component of the healthcare workforce and often serve as the primary point of contact for patients.
RNs are crucial for ensuring continuity of care, coordinating between different specialists, departments, and care settings. They interpret patient needs, advocate for appropriate treatments, and monitor patient progress closely. Their assessments and interventions directly influence patient outcomes and overall quality of care.
Modern nursing also involves leadership, research, and policy advocacy. Experienced RNs often manage nursing units, contribute to healthcare administration, conduct research to improve practice, and influence health policy at local, state, and national levels. Their frontline experience provides invaluable insights into the practical challenges and opportunities within healthcare delivery.
Understanding how healthcare systems function, including economic and delivery models, can provide valuable context for an RN's role. Many resources, like those found when browsing Health & Medicine courses on OpenCourser, delve into these topics.
Registered Nurse: Roles and Specializations
Clinical vs. Non-Clinical Pathways
Registered Nursing offers a wide array of career paths, broadly categorized into clinical and non-clinical roles. Clinical roles involve direct patient interaction and care. This is the most common image of nursing, encompassing bedside care in hospitals, administering treatments in clinics, or providing home health services.
Non-clinical roles leverage nursing knowledge and experience away from direct patient care. These paths can include nursing administration (managing nursing staff and operations), nursing education (teaching future nurses), health informatics (managing health data and systems), research (advancing nursing science), and public health policy.
Many RNs transition between clinical and non-clinical roles throughout their careers. Experience gained in direct patient care often provides a strong foundation for success in administrative, educational, or informatics positions. This flexibility allows RNs to adapt their careers to changing interests and life circumstances.
Exploring Common Nursing Specializations
Within clinical nursing, RNs can specialize in numerous areas, focusing on specific patient populations, diseases, or care settings. Pediatric nursing involves caring for infants, children, and adolescents. Critical care nurses work in intensive care units (ICUs), managing critically ill patients with complex needs.
Oncology nurses specialize in caring for patients with cancer, administering chemotherapy, managing symptoms, and providing emotional support. Geriatric nurses focus on the health needs of older adults. Other common specializations include emergency nursing, obstetrics (labor and delivery), psychiatric nursing, and surgical nursing.
Choosing a specialization often requires additional training, experience, and sometimes certification. Specializing allows RNs to develop deep expertise in a particular area, leading to greater professional satisfaction and potentially higher earning potential. OpenCourser features courses covering foundational knowledge relevant to many specialties, such as biology and physiology.
Emerging Frontiers in Nursing
The field of nursing is constantly evolving, with new roles and specializations emerging in response to technological advancements and changing healthcare needs. Telehealth nursing is rapidly growing, allowing RNs to provide care, monitoring, and education remotely using technology.
Nursing informatics combines nursing science with information management and analytical sciences to manage health data, improve patient care technologies like Electronic Health Records (EHR), and support clinical decision-making. Genetics nursing is another expanding field, focusing on assessing genetic risks and providing counseling related to inherited conditions.
Other emerging areas include forensic nursing (caring for victims of violence and collecting evidence), environmental health nursing (addressing health issues related to environmental factors), and holistic nursing (emphasizing mind-body-spirit connections in care). These evolving niches offer exciting opportunities for RNs interested in pioneering new approaches to healthcare.
These courses explore the growing field of health informatics and the use of technology in healthcare settings.
Formal Education Pathways
Degrees in Nursing: ADN vs. BSN
To become a Registered Nurse, individuals typically pursue either an Associate Degree in Nursing (ADN) or a Bachelor of Science in Nursing (BSN). An ADN program usually takes two to three years to complete and is often offered at community colleges. It provides the fundamental knowledge and clinical skills required for entry-level nursing practice and eligibility for the NCLEX-RN exam.
A BSN program generally takes four years at a university or college. It offers a broader education, including courses in nursing theory, research, leadership, and community health, in addition to clinical skills. While both ADN and BSN graduates can become licensed RNs, many healthcare organizations prefer BSN-prepared nurses, particularly for leadership roles or specialized positions.
The choice between ADN and BSN often depends on factors like time commitment, cost, and long-term career goals. Many RNs start with an ADN and later complete an RN-to-BSN bridge program, often available online, to advance their education and career opportunities.
Understanding the human body is crucial for any nursing path. Foundational courses in anatomy and physiology are essential.
Accelerated and Bridge Programs
For individuals who already hold a bachelor's degree in a field other than nursing, Accelerated BSN (ABSN) programs offer a faster path to becoming an RN. These intensive programs typically take 12 to 18 months to complete, building on the student's existing undergraduate education.
Similarly, bridge programs exist for Licensed Practical Nurses (LPNs) or Licensed Vocational Nurses (LVNs) who wish to become RNs. LPN-to-ADN or LPN-to-BSN programs provide a streamlined pathway by giving credit for prior nursing education and experience. These options recognize existing knowledge and facilitate career advancement.
These alternative pathways are rigorous and demand significant commitment but provide efficient routes into the RN profession for qualified individuals seeking a career change or advancement. Exploring options on platforms like OpenCourser can help identify preparatory courses in foundational sciences.
Clinical Experience: Rotations and Practicums
A critical component of any nursing education program is clinical experience, often referred to as clinical rotations or practicums. These supervised hands-on experiences allow students to apply theoretical knowledge in real-world healthcare settings, such as hospitals, clinics, and community health centers.
During clinical rotations, students work directly with patients under the guidance of experienced RNs and faculty instructors. They practice essential nursing skills, learn to navigate clinical environments, develop critical thinking and decision-making abilities, and gain exposure to various specialties.
The amount and type of clinical experience vary by program but are essential for developing competence and confidence as a nurse. These experiences are crucial preparation for the challenges and responsibilities of professional nursing practice and are required for licensure.
These courses provide insights into essential clinical skills and concepts that students encounter during rotations.
Advanced Nursing Education
For RNs seeking to advance their careers, specialize further, or move into leadership, education, or research roles, graduate degrees offer numerous opportunities. The Master of Science in Nursing (MSN) is a common pathway for becoming an Advanced Practice Registered Nurse (APRN).
APRN roles include Nurse Practitioners (NPs), Certified Registered Nurse Anesthetists (CRNAs), Clinical Nurse Specialists (CNSs), and Certified Nurse-Midwives (CNMs). These roles involve greater autonomy, diagnostic and prescribing authority (varying by state), and specialized expertise. MSN programs also prepare nurses for roles in administration, informatics, and education.
The Doctor of Nursing Practice (DNP) is a practice-focused doctorate, preparing nurses for leadership roles in clinical practice, administration, and policy. The Doctor of Philosophy (PhD) in Nursing is research-focused, preparing nurses for careers in academia and scientific investigation. Pursuing advanced education requires significant commitment but opens doors to highly specialized and influential roles within healthcare.
Licensing and Certification
The NCLEX-RN Examination
After completing an accredited nursing program (ADN or BSN), graduates must pass the National Council Licensure Examination for Registered Nurses (NCLEX-RN) to obtain their RN license. This standardized exam assesses the knowledge, skills, and abilities essential for safe and effective entry-level nursing practice.
The NCLEX-RN uses computerized adaptive testing (CAT), meaning the difficulty of questions adjusts based on the candidate's previous answers. The exam covers topics such as safe and effective care environment, health promotion and maintenance, psychosocial integrity, and physiological integrity. Thorough preparation is crucial for success.
Passing the NCLEX-RN is a mandatory step in every U.S. state and territory to become a licensed RN. Many resources, including review courses and practice tests, are available to help candidates prepare for this critical examination. OpenCourser offers resources in the Test Prep category that might assist.
State Licensure Requirements
In addition to passing the NCLEX-RN, candidates must meet specific requirements set by the Board of Nursing in the state where they intend to practice. These requirements typically include submitting proof of graduation from an approved nursing program, passing a criminal background check, and paying application fees.
RN licenses must be periodically renewed, usually every two to three years. Renewal often requires completing a certain number of continuing education hours to ensure nurses stay current with evolving practices and knowledge. Specific requirements vary by state.
The Nurse Licensure Compact (NLC) allows RNs licensed in a participating state to practice in other NLC member states without obtaining additional licenses. This facilitates mobility for nurses, particularly for travel nursing or practicing near state borders. Checking the specific requirements of your state's Board of Nursing is essential.
Specialty Certifications
While RN licensure demonstrates entry-level competence, specialty certifications validate advanced knowledge and skills in a specific area of nursing practice. Numerous certifications are available through various professional nursing organizations, covering fields like critical care (CCRN), emergency nursing (CEN), oncology (OCN), pediatrics (CPN), and many others.
Obtaining a specialty certification typically requires meeting specific eligibility criteria, such as a minimum number of practice hours in the specialty, holding an active RN license, and passing a certification exam. Certification demonstrates a commitment to professional development and expertise.
While not always mandatory for employment, specialty certifications can enhance career prospects, potentially lead to higher salaries, and signify a high level of competence and dedication within a chosen field. They are a valuable credential for RNs seeking to advance in specialized roles.
These courses touch upon specialized areas where certification might be pursued, such as palliative care or emergency response.
Lifelong Learning: Continuing Education
Nursing is a dynamic field with continuous advancements in medical knowledge, technology, and best practices. Consequently, lifelong learning through continuing education (CE) is essential for maintaining competence and providing high-quality care. Most state Boards of Nursing mandate a specific number of CE hours for license renewal.
CE activities can include attending workshops, conferences, online courses, or reading professional journals. Topics range widely, covering clinical updates, new treatment modalities, ethical considerations, technological advancements, and changes in healthcare regulations. CE ensures that RNs remain current in their knowledge and skills.
Beyond meeting licensure requirements, engaging in ongoing learning supports professional growth, enhances critical thinking, and can open doors to new opportunities or specialized roles. Platforms like OpenCourser offer a vast catalog of courses relevant for CE, covering topics from basic life support refreshers to advanced clinical concepts. The OpenCourser Learner's Guide provides tips on maximizing learning from online resources.
These courses cover important areas like medication updates and managing specific conditions, relevant for continuing education.
Career Progression for Registered Nurses
Climbing the Clinical Ladder
Many RNs begin their careers as staff nurses, providing direct patient care in various settings. With experience, they can advance along a clinical ladder. This might involve becoming a preceptor (mentoring new nurses), a charge nurse (overseeing a nursing unit during a shift), or a clinical nurse specialist (providing expert consultation within a specialty).
Further advancement can lead to roles like nurse manager or assistant nurse manager, responsible for overseeing the operations, staffing, and budget of a specific unit or department. Higher-level administrative positions, such as Director of Nursing or Chief Nursing Officer (CNO), involve broader leadership responsibilities across an entire facility or healthcare system.
This progression typically requires additional education (often a BSN or MSN), demonstrated leadership skills, and significant clinical experience. The clinical ladder provides a structured pathway for RNs to increase their responsibility, influence, and compensation while remaining closely connected to clinical practice or operations.
Becoming an Advanced Practice Registered Nurse (APRN)
Pursuing graduate education (MSN or DNP) opens the door to Advanced Practice Registered Nurse (APRN) roles. Nurse Practitioners (NPs) provide primary, acute, or specialty care, often with diagnostic and prescribing authority. They work in diverse settings, sometimes independently, managing patient health across the lifespan.
Certified Registered Nurse Anesthetists (CRNAs) administer anesthesia for surgical, diagnostic, and therapeutic procedures. Clinical Nurse Specialists (CNSs) provide expert clinical guidance, education, and research within a specific population or setting. Certified Nurse-Midwives (CNMs) offer comprehensive care to women, including prenatal, labor/delivery, and postpartum care, as well as gynecological services.
APRN roles represent a significant expansion of scope and responsibility compared to traditional RN roles. They require advanced clinical skills, critical thinking, and leadership abilities, offering highly rewarding and autonomous career paths within nursing.
Beyond the Bedside: Alternative Nursing Careers
An RN's skills and experience are valuable in many settings outside direct patient care. Nurses can transition into roles in healthcare informatics, managing and analyzing health data to improve care delivery and system efficiency. Nursing education offers opportunities to teach in academic institutions or provide staff development within healthcare organizations.
Research nursing involves conducting clinical trials or studies to advance medical knowledge and nursing practice. Public health nurses work in communities, focusing on health promotion, disease prevention, and addressing population health needs. Opportunities also exist in healthcare administration, policy development, legal nurse consulting, and case management.
These alternative paths allow RNs to leverage their clinical background in diverse ways, contributing to healthcare from different perspectives. They often require additional education or certification but offer flexibility and the chance to impact health on a broader scale.
This book provides insights into the administrative side of healthcare.
Workplace Settings and Environments
Diverse Healthcare Settings
Registered Nurses practice in a remarkably wide range of settings. Hospitals remain the largest employers, offering opportunities in various units like emergency rooms, ICUs, operating rooms, medical-surgical floors, and maternity wards. Each hospital unit presents unique challenges and patient populations.
Beyond hospitals, RNs work in outpatient clinics, physician offices, and ambulatory surgery centers, often focusing on preventative care, chronic disease management, and minor procedures. Long-term care facilities, including nursing homes and rehabilitation centers, employ RNs to care for elderly or disabled residents.
RNs also work in schools, providing health services to students; in home healthcare agencies, visiting patients in their homes; in correctional facilities; in military bases; and in public health departments, focusing on community wellness. This variety allows nurses to find environments that align with their interests and lifestyle preferences.
Unique Opportunities: Travel and Agency Nursing
Travel nursing offers RNs the opportunity to take temporary assignments, typically lasting 8-13 weeks, in different hospitals or healthcare facilities across the country or even internationally. These roles often come with higher pay rates, housing stipends, and the chance to experience diverse clinical settings and locations.
Agency nursing involves working for a staffing agency that places nurses in facilities needing temporary coverage, often on a per diem (day-to-day) or short-term contract basis. This provides flexibility in scheduling and exposure to different workplaces.
Both travel and agency nursing require adaptability, strong clinical skills, and the ability to quickly integrate into new teams and environments. They are attractive options for nurses seeking flexibility, higher compensation, and varied experiences, though they may lack the stability and benefits of permanent positions.
Nursing in Corporate and Occupational Health
RNs also find roles within corporations and various workplaces as occupational health nurses. Their focus is on promoting employee health and safety, preventing workplace injuries and illnesses, and managing work-related health issues. This can involve conducting health screenings, providing first aid, developing wellness programs, and ensuring compliance with safety regulations.
Some large companies employ nurses in corporate wellness programs or on-site clinics to provide convenient healthcare access for employees. Insurance companies hire RNs for case management, utilization review, or disease management programs, helping patients navigate their care and ensuring appropriate use of resources.
These roles often offer more traditional business hours compared to clinical settings. They require strong communication skills, knowledge of workplace safety principles, and the ability to apply nursing expertise in a non-traditional healthcare environment.
Essential Skills and Competencies
Mastering Clinical Skills
Proficiency in a wide range of clinical skills is fundamental to nursing practice. This includes conducting thorough patient assessments, accurately measuring vital signs, and interpreting findings to inform care plans. Technical skills like administering medications (oral, injectable, intravenous), inserting IV lines, performing wound care, and managing medical equipment are essential.
RNs must be adept at recognizing changes in a patient's condition and responding appropriately, often in high-pressure situations. They need to understand disease processes, diagnostic procedures, and treatment protocols across various medical conditions. Mastery of these skills requires rigorous training, ongoing practice, and a commitment to precision.
Many online courses offer refreshers or introductions to specific clinical skills and concepts, helping both students and practicing nurses maintain their proficiency.
These courses cover vital clinical skills and assessments necessary for RNs.
The Power of Soft Skills
While clinical competence is crucial, effective nursing equally relies on strong soft skills. Communication is paramount – RNs must clearly convey information to patients, families, and other healthcare team members. Active listening and therapeutic communication techniques help build trust and understand patient concerns.
Empathy, the ability to understand and share the feelings of others, is vital for providing compassionate care. Critical thinking allows nurses to analyze complex situations, prioritize tasks, and make sound clinical judgments. Problem-solving skills are needed to address unexpected issues and adapt care plans as needed.
Teamwork and collaboration are essential, as nurses work closely with physicians, therapists, and other staff. Resilience, stress management, and emotional intelligence help nurses navigate the demanding and often emotionally charged aspects of the profession. Developing these interpersonal skills is as important as mastering technical procedures.
These courses focus on developing crucial soft skills like communication and resilience, which are vital for nursing success.
Navigating Health Technology
Modern healthcare relies heavily on technology, and RNs must be proficient in using various digital tools. Electronic Health Record (EHR) systems are standard in most settings for documenting patient care, accessing medical histories, and communicating with the care team. Familiarity with EHR navigation and accurate documentation is critical.
Nurses operate sophisticated medical devices, such as infusion pumps, cardiac monitors, and ventilators, requiring technical understanding and troubleshooting skills. Telehealth platforms are increasingly used for remote patient monitoring and virtual consultations, demanding comfort with video conferencing and digital communication tools.
Basic computer literacy and the ability to adapt to new software and devices are essential. As technology continues to evolve, nurses must engage in ongoing learning to effectively utilize new tools that enhance patient care, improve efficiency, and ensure patient safety.
Challenges and Occupational Risks
Physical Demands of Nursing
Nursing is physically demanding work. RNs spend long hours on their feet, often walking several miles during a single shift. The job frequently involves lifting and repositioning patients, which can strain the back and joints if proper body mechanics are not used.
Shift work, including nights, weekends, and holidays, is common, especially in hospital settings. Irregular schedules can disrupt sleep patterns and impact personal life. The fast-paced nature of many nursing roles requires stamina and the ability to sustain energy levels throughout demanding shifts.
While rewarding, the physical toll is a significant aspect of the career. Maintaining personal fitness, using assistive devices for lifting, and advocating for safe staffing levels are important strategies for mitigating these physical demands.
Emotional Toll and Burnout
Nursing can be emotionally taxing. RNs frequently care for patients experiencing pain, fear, and loss. Witnessing suffering and dealing with difficult diagnoses or outcomes can lead to emotional distress and compassion fatigue over time.
High-stress work environments, heavy workloads, staffing shortages, and dealing with challenging patient or family interactions contribute to the risk of burnout. Burnout is characterized by emotional exhaustion, depersonalization (feeling detached from one's work or patients), and a reduced sense of personal accomplishment.
Recognizing the signs of burnout and practicing self-care are crucial. Strategies include seeking peer support, utilizing employee assistance programs, setting boundaries, engaging in stress-reducing activities like mindfulness or exercise, and taking adequate time off. Addressing systemic issues like workload and staffing is also vital for preventing widespread burnout. Resources from organizations like the CDC offer guidance on workplace stress in healthcare.
These resources focus on mental well-being and managing the emotional challenges inherent in healthcare roles.
Workplace Hazards
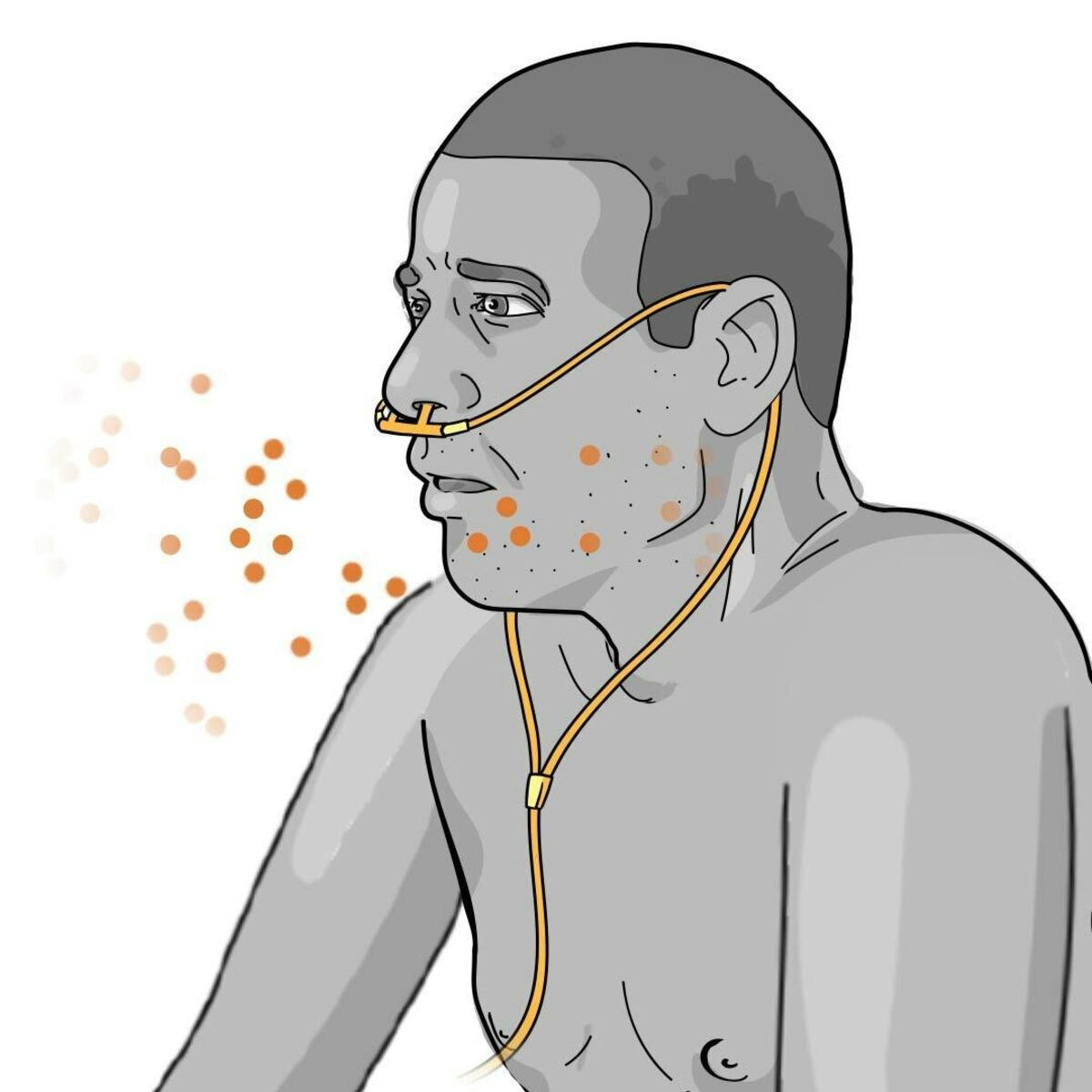
RNs face various occupational hazards in their work environments. Exposure to infectious diseases is a significant risk, requiring strict adherence to infection control protocols, use of personal protective equipment (PPE), and vaccinations. Needlestick injuries can expose nurses to bloodborne pathogens like HIV and Hepatitis C.
Exposure to hazardous chemicals, medications (like chemotherapy drugs), and radiation are potential risks in certain settings. Workplace violence, including verbal abuse and physical assault from patients or visitors, is an unfortunate reality in healthcare that requires preventative measures and safety training.
Healthcare facilities implement safety protocols and provide training to minimize these risks. However, vigilance, proper use of safety equipment, and adherence to procedures are essential for protecting oneself from workplace hazards.
These courses cover infection control and safety measures crucial in healthcare settings.
Strategies for Well-being and Risk Mitigation
Given the demanding nature of the job, proactive strategies for well-being are essential for a sustainable nursing career. Prioritizing self-care, including adequate sleep, healthy nutrition, regular exercise, and engaging in hobbies outside of work, helps build resilience.
Utilizing workplace resources such as employee assistance programs (EAPs), peer support groups, and debriefing sessions after critical incidents can provide valuable emotional support. Practicing mindfulness and stress-reduction techniques can help manage daily pressures.
Strict adherence to safety protocols, including proper use of PPE, safe lifting techniques, and reporting hazardous conditions, is crucial for mitigating physical risks. Advocating for safe staffing levels and supportive work environments also contributes to overall well-being and reduces occupational hazards for all healthcare workers.
Industry Trends Impacting Registered Nurses
Addressing the Nursing Shortage
Many regions, including the U.S., face persistent nursing shortages. Factors contributing to this include an aging nursing workforce, increasing demand for healthcare services due to an aging population and rising rates of chronic diseases, and challenges in nursing education capacity.
The U.S. Bureau of Labor Statistics projects strong job growth for RNs over the next decade, indicating continued high demand. This shortage puts pressure on existing nurses, potentially leading to higher workloads and burnout, but also creates numerous job opportunities and potential for competitive compensation and benefits.
Efforts to address the shortage include initiatives to expand nursing school enrollment, improve retention rates through better work environments and support systems, and explore innovative care delivery models that optimize nursing roles.
Technology's Role: AI and Automation
Technological advancements, including Artificial Intelligence (AI) and automation, are increasingly influencing nursing practice. AI can assist with tasks like analyzing medical images, predicting patient deterioration, and optimizing staffing schedules. Automation may handle routine tasks like medication dispensing or sample transport.
These technologies have the potential to enhance efficiency, reduce errors, and free up nurses' time for more complex clinical reasoning and direct patient interaction. However, they also raise questions about changes in workflow, the need for new skills (like data interpretation), and potential impacts on the nurse-patient relationship.
RNs will need to adapt to and collaborate with these technologies. Continuous learning and embracing digital literacy will be crucial for navigating the evolving technological landscape in healthcare.
Global Health and Preparedness
Recent global health events, particularly the COVID-19 pandemic, have highlighted the critical role of nurses in public health surveillance, infectious disease control, and emergency preparedness. RNs are on the front lines during health crises, providing direct care, administering vaccines, educating the public, and adapting to rapidly changing protocols.
This increased focus on global health and pandemic preparedness influences nursing education, practice standards, and policy. There is a growing emphasis on skills related to infection control, disaster response, public health principles, and understanding the social determinants of health that impact vulnerability during crises.
Nurses with expertise in global health, epidemiology, and emergency management are increasingly valuable. Understanding these broader contexts helps RNs contribute effectively to community and global health initiatives.
These courses offer insights into pandemic response and global health challenges, increasingly relevant areas for nurses.
Labor Issues and Advocacy
Working conditions, staffing levels, scope of practice, and compensation are ongoing areas of discussion and advocacy within the nursing profession. Nursing unions and professional organizations play significant roles in negotiating contracts, lobbying for legislation, and promoting policies that support nurses and patient safety.
Issues such as mandatory overtime, safe nurse-to-patient ratios, and workplace violence prevention are key areas of focus for labor advocacy. Discussions around expanding the scope of practice for APRNs also continue, varying significantly by state regulations.
Understanding these labor trends and the role of professional advocacy is important for RNs. Engaging with professional organizations or unions allows nurses to have a collective voice in shaping their work environment and the future of the profession.
Frequently Asked Questions (FAQs)
What is the typical salary range for an RN?
Registered Nurse salaries vary considerably based on geographic location, years of experience, education level (ADN vs. BSN vs. MSN/DNP), specialty certification, and type of employer. Urban areas and states with higher costs of living generally offer higher salaries.
According to the U.S. Bureau of Labor Statistics, the median annual wage for registered nurses was $86,070 in May 2023. However, this is just a midpoint; entry-level salaries will be lower, while experienced nurses in high-demand specialties or management roles can earn significantly more.
Factors like shift differentials (extra pay for evening, night, or weekend shifts), overtime opportunities, and benefits packages also contribute to overall compensation. Researching salary data specific to your region and desired specialty is recommended.
Can I advance my career without leaving direct patient care?
Absolutely. While some advancement paths lead away from the bedside (like administration or education), many opportunities exist for career growth while remaining in direct patient care. Achieving specialty certifications allows RNs to become recognized experts in fields like critical care, oncology, or pediatrics, often leading to roles with more autonomy or higher pay.
Many hospitals have clinical ladder programs that allow nurses to advance to higher levels (e.g., Clinical Nurse II, III, IV) based on experience, skills, education, and contributions like mentoring or quality improvement projects. These advanced clinical roles often involve more complex patient assignments or leadership responsibilities within the care team.
Becoming an Advanced Practice Registered Nurse (APRN), such as a Nurse Practitioner or Clinical Nurse Specialist, is another way to advance significantly while maintaining a strong focus on direct patient care, albeit with an expanded scope of practice.
How easy is it to switch between nursing specialties?
Switching between nursing specialties is common and feasible, though the ease varies depending on the specialties involved and the nurse's experience. Transitioning often requires acquiring new knowledge and skills specific to the new area. This might involve on-the-job training, formal orientation programs, continuing education courses, or even obtaining a new specialty certification.
Some transitions are relatively smooth, particularly between related fields (e.g., medical-surgical to telemetry). Moving to highly specialized areas like the ICU, operating room, or labor and delivery typically requires more intensive training and may be more competitive to enter.
Employers often look for relevant experience or demonstrated interest when hiring for specialized roles. Networking, shadowing nurses in the desired specialty, and taking relevant CE courses can facilitate a successful transition. The adaptability and broad foundational knowledge of RNs make career pivots within the profession achievable.
What are the options for part-time or PRN (as needed) work?
Nursing offers significant flexibility regarding work schedules, including part-time and PRN (pro re nata, meaning "as needed") options. Many hospitals and healthcare facilities hire part-time RNs who work fewer hours per week than full-time staff, often with pro-rated benefits.
PRN or per diem roles involve working on an as-needed basis to fill staffing gaps, cover vacations, or manage fluctuating patient volumes. PRN nurses typically have more control over their schedules but usually do not receive benefits like health insurance or paid time off. They often earn a higher hourly wage to compensate for the lack of benefits and schedule unpredictability.
These flexible options are attractive for nurses seeking better work-life balance, pursuing further education, managing family responsibilities, or semi-retiring. The availability of part-time and PRN positions varies by employer and geographic location.
What is the job outlook for RNs in the next decade?
The job outlook for Registered Nurses remains very strong. The U.S. Bureau of Labor Statistics projects employment of RNs to grow 6 percent from 2022 to 2032, about as fast as the average for all occupations.
This growth is driven by several factors, including an aging population requiring more healthcare services, increased emphasis on preventative care, and rising rates of chronic conditions like diabetes and obesity. Additionally, many nurses from the baby boomer generation are retiring, creating further job openings.
Demand is expected across various healthcare settings, including hospitals, outpatient care centers, and long-term care facilities. Nurses with advanced degrees (BSN or higher) and specialty certifications will likely have the best job prospects.
What's the difference between an RN, LPN/LVN, and CNA?
RNs, LPNs/LVNs (Licensed Practical/Vocational Nurses), and CNAs (Certified Nursing Assistants) are all vital members of the healthcare team, but they differ in their scope of practice, education requirements, and responsibilities.
CNAs provide basic patient care under the supervision of RNs or LPNs. Their duties typically include assisting with activities of daily living (bathing, dressing, feeding), taking vital signs, and reporting changes to nurses. CNA training programs are relatively short, often completed in a few weeks or months.
LPNs/LVNs provide more comprehensive care than CNAs but work under the direction of RNs or physicians. Their scope includes administering certain medications, monitoring patients, and performing basic nursing tasks. LPN/LVN programs typically take about one year to complete. RNs have the broadest scope of practice, involving complex assessments, care planning, administration of all types of medications, patient education, and often supervision of LPNs and CNAs. RN education requires an ADN (2-3 years) or BSN (4 years).
Helpful Resources and Next Steps
Embarking on or advancing a career in registered nursing involves continuous learning and accessing reliable resources. Professional organizations offer valuable support, networking opportunities, and continuing education.
- American Nurses Association (ANA): The premier organization representing the interests of the nation's registered nurses. (www.nursingworld.org)
- National League for Nursing (NLN): Focuses on excellence in nursing education. (www.nln.org)
- State Boards of Nursing: Each state has its own board responsible for licensing and regulation. Search for your specific state's board for detailed requirements.
- Specialty Nursing Organizations: Numerous organizations exist for specific areas (e.g., American Association of Critical-Care Nurses - AACN, Oncology Nursing Society - ONS).
- OpenCourser: Explore thousands of courses related to Health & Medicine, including anatomy, physiology, pharmacology, and specialized nursing topics to build foundational knowledge or meet continuing education needs.
Utilizing these resources can help aspiring and current nurses navigate their educational path, licensure process, and ongoing professional development.
A career as a Registered Nurse is challenging, requiring intellectual rigor, physical stamina, and deep emotional resilience. However, it offers the profound reward of making a direct, positive impact on the health and well-being of individuals and communities. With diverse pathways, specialization options, and strong job prospects, nursing provides a stable and meaningful lifelong profession. If you are considering this path, further exploration through resources like OpenCourser can help you prepare for the journey ahead.