Nurse Practitioner
Comprehensive Guide to a Career as a Nurse Practitioner
A Nurse Practitioner (NP) is an advanced practice registered nurse (APRN) who has completed graduate-level education, such as a Master of Science in Nursing (MSN) or a Doctor of Nursing Practice (DNP). This advanced training prepares NPs to provide a wide range of healthcare services, including diagnosing and treating acute and chronic illnesses, ordering and interpreting diagnostic tests, prescribing medications, and managing overall patient care. NPs often focus on health promotion, disease prevention, and patient education, offering a holistic approach to healthcare. Millions of people choose NPs as their primary healthcare providers.
Working as a Nurse Practitioner can be incredibly engaging and exciting. One of the key aspects is the ability to make a significant impact on patients' lives by providing comprehensive care and building long-term relationships. The role also offers a high degree of autonomy, with many NPs managing their own patient panels and, in some states, even owning their own practices. Furthermore, the field is constantly evolving, presenting opportunities to specialize in diverse areas such as pediatrics, mental health, or gerontology, ensuring a dynamic and intellectually stimulating career.
Introduction to Nurse Practitioners
This section will delve into the specifics of what it means to be a Nurse Practitioner, exploring the historical context of the profession and clarifying how this role differs from other vital healthcare positions.
Defining the Nurse Practitioner Role and Scope
Nurse Practitioners are advanced practice registered nurses (APRNs) who are educated at the master's or doctoral level. Their scope of practice is broad and involves assessing patients, ordering and interpreting diagnostic tests, making diagnoses, and initiating and managing treatment plans, which includes prescribing medications and non-pharmacologic therapies. NPs emphasize health promotion and disease prevention and provide patient counseling and education. They practice in a multitude of settings, such as clinics, hospitals, private practices, and public health departments. Depending on state regulations, NPs may practice autonomously or in collaboration with other healthcare professionals.
The NP role is distinct due to its patient-centered nature, requiring a commitment to the evolving needs of society and advancements in healthcare. NPs often act as providers, mentors, educators, researchers, advocates, and administrators. Their responsibilities extend to continued professional development and participation in health policy. The focus of an NP's practice is determined by patient needs and is not confined to a specific setting.
For individuals considering this career, understanding the depth and breadth of an NP's responsibilities is crucial. It's a demanding yet rewarding profession that blends clinical expertise with a strong focus on patient well-being and preventative care. The ability to manage complex health problems while also guiding patients towards healthier lifestyles is a hallmark of the NP role.
To gain a foundational understanding of the healthcare environment and patient care, some introductory courses could be beneficial. These courses can help you explore core concepts in medicine and healthcare delivery.
Exploring texts on health equity and the social determinants of health can provide a broader context for the NP's role in addressing diverse patient needs.
Historical Development of the NP Profession
The Nurse Practitioner profession originated in the United States in 1965 at the University of Colorado. This development was largely in response to a shortage of physicians, particularly in primary care and in rural or underserved areas. The initial programs aimed to expand the role of nurses to help fill these gaps in healthcare access.
Initially, there was resistance to the NP role, with concerns about the adequacy of their training compared to physicians. However, over the decades, numerous studies have affirmed the safety, quality, and cost-effectiveness of NP-provided care. This growing body of evidence, coupled with the continued need for accessible healthcare, has led to the expansion and wider acceptance of the NP profession.
State laws and regulations governing NP practice have evolved significantly since the 1970s. While some states now grant NPs full practice authority, allowing them to operate independently, others maintain more restrictive regulations requiring physician oversight or collaboration. The journey towards national standardization of NP scope of practice continues to be a key focus for professional organizations.
Key Distinctions: NPs, RNs, and Physicians
Understanding the differences between Nurse Practitioners (NPs), Registered Nurses (RNs), and Physicians (MDs or DOs) is essential for anyone considering a career in healthcare. While all three roles are vital to patient care, they differ significantly in terms of education, scope of practice, and responsibilities.
Registered Nurses typically hold an associate's degree in nursing (ADN) or a Bachelor of Science in Nursing (BSN). Their primary focus is on direct patient care, implementing treatment plans prescribed by physicians or NPs, administering medications (as ordered), educating patients, and monitoring patient conditions. RNs work under the supervision of physicians or more senior nurses and do not typically have diagnostic or prescriptive authority.
Nurse Practitioners, on the other hand, are RNs who have completed advanced graduate-level education (an MSN or DNP). This additional education and clinical training equip them with the skills to diagnose illnesses, develop and manage treatment plans, order and interpret diagnostic tests, and prescribe medications. NPs often function as primary care providers and, in many states, can practice independently without direct physician oversight. Their approach often emphasizes health promotion, disease prevention, and a holistic view of patient well-being.
Physicians (MDs - Medical Doctors or DOs - Doctors of Osteopathic Medicine) complete medical school followed by several years of residency training in a specific specialty. Their education is the most extensive, providing them with the broadest scope of practice, including diagnosing and treating complex medical conditions and performing surgical procedures. While NPs can manage many common and chronic health problems, physicians often handle more complex or specialized cases. The training for physicians involves significantly more patient-care hours compared to NPs.
For those exploring these career paths, it's important to recognize that while there is overlap in some functions, especially between NPs and physicians in primary care settings, the educational pathways, legal scopes of practice, and ultimate levels of autonomy and responsibility are distinct. Choosing between these roles depends on individual career aspirations, desired level of autonomy, and the kind of patient interaction and care one wishes to provide.
To further understand the foundational aspects of nursing and the healthcare system, these courses can be insightful.
Nurse Practitioner Roles and Responsibilities
Nurse Practitioners fulfill a wide array of critical functions within the healthcare system. Their responsibilities span from direct patient care to collaborative efforts within larger healthcare teams, all aimed at improving patient outcomes and promoting health.
Primary Care versus Specialty Practice Domains
Nurse Practitioners can choose to work in primary care or specialize in a particular area of medicine. Primary care NPs provide comprehensive, ongoing healthcare to individuals and families across all ages. They manage common illnesses, promote health, prevent diseases, and coordinate patient care. The American Association of Nurse Practitioners (AANP) highlights that over 88% of NPs are educated in primary care, and a significant majority of them deliver primary care services.
Specialty practice NPs focus on a specific patient population or medical area, such as pediatrics, women's health, psychiatric-mental health, adult-gerontology, or neonatal care. They may also specialize in acute care, cardiology, dermatology, oncology, or emergency medicine. These NPs develop in-depth expertise in their chosen field, managing complex health issues related to that specialty. The scope of practice for both primary care and specialty NPs is determined by their education, certification, and state licensure.
The decision to pursue primary care or a specialty often depends on an NP's interests, career goals, and the patient populations they wish to serve. Both pathways offer rewarding opportunities to make a significant impact on patient health and well-being.
For those interested in the breadth of primary care or the depth of specialty practice, exploring relevant online courses can provide valuable insights. These courses cover a range of topics from managing common conditions to understanding specific patient populations.
Books focusing on specific areas of health or patient populations can also deepen understanding.
Diagnostic Authority and Prescriptive Privileges
A key aspect of the Nurse Practitioner role is their authority to diagnose health conditions and prescribe medications. This authority is granted through state licensure and is a significant differentiator from the role of a Registered Nurse. NPs are trained to perform comprehensive health assessments, order and interpret diagnostic tests (such as lab work and imaging), and formulate diagnoses based on these findings.
Prescriptive privileges allow NPs to prescribe a wide range of medications, including controlled substances in many jurisdictions. The extent of these privileges, including the types of medications NPs can prescribe and the degree of physician collaboration or supervision required, varies significantly by state. According to the AANP, NPs hold prescriptive authority in all 50 states and the District of Columbia. Some states grant "full practice authority," where NPs can diagnose, treat, and prescribe independently, while others have "reduced" or "restricted" practice environments requiring varying levels of physician involvement.
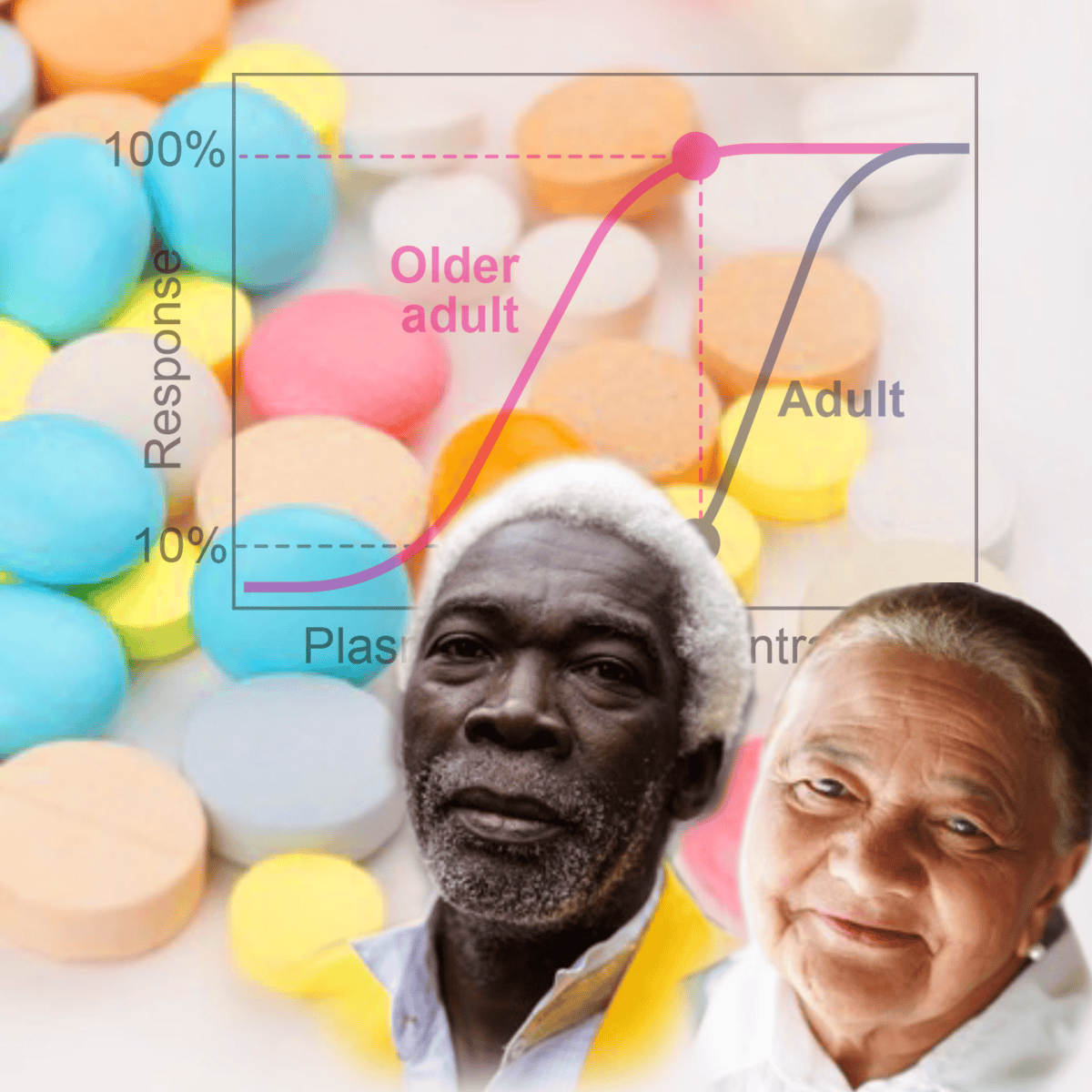
The ability to diagnose and prescribe is fundamental to an NP's capacity to provide comprehensive patient care and manage both acute and chronic conditions effectively. This authority comes with significant responsibility, requiring NPs to maintain up-to-date knowledge of pharmacology, diagnostic procedures, and evidence-based treatment guidelines. Ongoing pharmacology continuing education is often a requirement for maintaining licensure and certification.
Courses focusing on pharmacology and diagnostics can provide a deeper understanding of these critical NP responsibilities.
Patient Education and Chronic Disease Management
Patient education and the management of chronic diseases are cornerstone responsibilities for Nurse Practitioners. NPs play a crucial role in empowering patients with the knowledge and skills to understand their health conditions, participate in their care, and make informed decisions about their treatment and lifestyle. This includes explaining diagnoses, treatment options, medication regimens, and potential side effects in an accessible manner.
In chronic disease management, NPs are instrumental in helping patients navigate long-term health challenges such as diabetes, hypertension, heart disease, asthma, and arthritis. They develop individualized care plans, monitor patient progress, adjust treatments as needed, and provide ongoing support and counseling. A significant part of this involves teaching self-management strategies, such as dietary modifications, exercise routines, symptom monitoring, and when to seek further medical attention. Studies have shown that NPs can be highly effective in improving patient outcomes in chronic disease management, including better control of conditions and reduced hospitalizations. Some research even suggests that PAs and NPs may provide health education to patients with chronic conditions at a higher rate than physicians.
The emphasis NPs place on health promotion and disease prevention is particularly valuable in managing chronic illnesses. By focusing on preventative measures and early intervention, NPs can help slow disease progression and improve the overall quality of life for their patients. This holistic and patient-centered approach is a defining characteristic of NP care.
Online courses focused on chronic conditions and patient communication can enhance skills in these vital areas.
Understanding the broader context of public health and patient interaction is also crucial.
Collaboration with Healthcare Teams
While Nurse Practitioners in many states can practice autonomously, collaboration with other healthcare professionals is a common and often essential aspect of their role. NPs work alongside physicians, specialists, registered nurses, pharmacists, social workers, physical therapists, and other members of the healthcare team to provide comprehensive and coordinated patient care. This interprofessional collaboration is vital for managing complex patient needs and ensuring optimal health outcomes.
Effective communication and teamwork are key to successful collaboration. NPs often serve as a crucial link between different providers, helping to coordinate care plans, share important patient information, and ensure that all aspects of a patient's health are addressed. They may consult with physicians on complex cases, refer patients to specialists when necessary, and work with allied health professionals to implement rehabilitative or supportive therapies.
The ability to work effectively within a team is a critical skill for NPs, regardless of their practice setting or level of autonomy. Healthcare is increasingly a team-based endeavor, and NPs who can foster strong working relationships with their colleagues are better positioned to advocate for their patients and contribute to a positive and efficient healthcare environment. This collaborative spirit also extends to research and policy development, where NPs often work with other professionals to advance healthcare practices and address systemic issues.
Courses that touch upon teamwork, communication, and healthcare systems can be beneficial for aspiring NPs.
Formal Education Pathways
Embarking on a career as a Nurse Practitioner involves a dedicated and structured educational journey. This section outlines the typical academic routes, from foundational undergraduate studies to advanced graduate programs, highlighting the rigorous training required.
Undergraduate Prerequisites (BSN Requirements)
The foundational step towards becoming a Nurse Practitioner is typically earning a Bachelor of Science in Nursing (BSN) degree. A BSN program usually takes four years to complete and provides comprehensive training in nursing theory, clinical skills, and sciences such as anatomy, physiology, pharmacology, and microbiology. This undergraduate education equips aspiring NPs with the fundamental knowledge and practical experience necessary for registered nursing practice.
In addition to a BSN, admission to an NP program requires an active and unencumbered Registered Nurse (RN) license. This means that after completing a BSN (or an Associate Degree in Nursing - ADN - followed by an RN-to-BSN bridge program), graduates must pass the National Council Licensure Examination for Registered Nurses (NCLEX-RN) to become licensed RNs. Many NP programs also have specific GPA requirements for undergraduate coursework, often a 3.0 or higher on a 4.0 scale. Some programs may also require prerequisite courses like statistics or nursing research.
For individuals considering a career change into nursing with the ultimate goal of becoming an NP, accelerated BSN programs or direct-entry MSN programs might be options if they already hold a bachelor's degree in another field. However, gaining experience as an RN before pursuing advanced practice education is often recommended and sometimes required.
Building a strong academic foundation during your undergraduate studies is crucial. Courses in anatomy, physiology, and general sciences are essential for success in advanced nursing programs.
Master's vs. Doctor of Nursing Practice (DNP) Programs
Once a BSN and RN licensure are obtained, aspiring Nurse Practitioners must pursue graduate-level education. The two primary degree options are the Master of Science in Nursing (MSN) and the Doctor of Nursing Practice (DNP). Both degrees prepare nurses for advanced practice roles, but there are key differences in their focus and length.
An MSN has traditionally been the standard degree for NP entry into practice. MSN programs typically take 18 months to three years to complete and provide specialized clinical training in a chosen population focus (e.g., family, pediatrics, adult-gerontology). The curriculum emphasizes advanced assessment, diagnosis, pharmacology, and management of health conditions.
The DNP is a terminal practice doctorate for nursing. DNP programs build upon MSN-level competencies, adding coursework in areas like evidence-based practice, quality improvement, systems leadership, health policy, and informatics. A DNP typically requires an additional year or more of study beyond an MSN, or can be pursued directly after a BSN in a BSN-to-DNP program, which often takes three to four years. While an MSN prepares NPs for clinical practice, the DNP is designed to prepare leaders in clinical practice, healthcare administration, and policy. There is a growing movement within the nursing profession to make the DNP the standard entry-level degree for NPs, with some organizations advocating for this change by 2025, although currently, an MSN still allows for NP certification and licensure.
Choosing between an MSN and a DNP depends on individual career goals. If the primary aim is direct clinical practice as an NP, an MSN may suffice. However, for those aspiring to leadership roles, positions in academia, or a desire to influence healthcare systems and policy, a DNP offers more extensive preparation. Both degrees lead to higher earning potential compared to a BSN.
Online courses that delve into evidence-based practice and healthcare leadership can provide a taste of DNP-level coursework.
Further reading on healthcare delivery and evaluation can provide context for the advanced roles NPs can play.
Clinical Hour Requirements by State
A critical component of Nurse Practitioner education is the completion of supervised clinical hours. These hours provide students with hands-on experience in their chosen specialty area, allowing them to apply their academic knowledge in real-world patient care settings under the guidance of experienced preceptors (who may be NPs or physicians).
The number of clinical hours required can vary depending on the specific NP program, the chosen specialty, and, significantly, the state in which the NP intends to practice. National accrediting bodies for NP programs, such as the Commission on Collegiate Nursing Education (CCNE) and the Accreditation Commission for Education in Nursing (ACEN), typically mandate a minimum number of clinical hours for program accreditation. For instance, many programs require at least 500-750 supervised clinical hours for an MSN, with DNP programs often requiring 1,000 hours or more. Physician training, for comparison, involves 12,000 to 16,000 hours of patient care experience between medical school and residency.
It is crucial for prospective NP students to research the specific clinical hour requirements not only of their desired educational program but also of the state board of nursing in the state(s) where they plan to seek licensure. Some states may have requirements that exceed the minimums set by accrediting bodies or individual programs. Failure to meet a state's specific clinical hour mandates can impede licensure, even if an NP has graduated from an accredited program and passed national certification exams.
Securing clinical placements can sometimes be a challenge for NP students, and it is important to inquire about how programs assist students in finding appropriate preceptors and sites. The quality and variety of clinical experiences are just as important as the total number of hours, as these experiences directly shape an NP's competence and confidence upon entering practice.
While direct clinical hours are irreplaceable, courses focusing on clinical reasoning and patient assessment can help build a strong theoretical foundation.
Accreditation Standards for NP Programs
Accreditation is a vital quality assurance process for Nurse Practitioner programs. It signifies that a program has met rigorous national standards for educational quality, curriculum, faculty, resources, and student outcomes. Prospective NP students should ensure that any program they consider is accredited by a recognized agency.
The primary accrediting bodies for NP programs in the United States are the Commission on Collegiate Nursing Education (CCNE) and the Accreditation Commission for Education in Nursing (ACEN). Both organizations are recognized by the U.S. Department of Education. Graduating from an accredited program is typically a prerequisite for taking national NP certification exams and for obtaining state licensure.
Accreditation standards ensure that NP programs provide a curriculum grounded in evidence-based practice and prepare graduates with the core competencies necessary for safe and effective advanced practice nursing. These competencies often align with models such as the APRN Consensus Model, which outlines expectations for APRN roles, education, licensure, certification, and regulation. Standards generally cover areas like curriculum content (including advanced pathophysiology, pharmacology, and physical assessment), clinical practice requirements, faculty qualifications, and program effectiveness measures (such as graduation rates, certification pass rates, and employment rates).
Attending a non-accredited program can severely limit a graduate's career options, as they may be ineligible for certification, licensure, and employment as an NP. Therefore, verifying a program's accreditation status is a critical early step in the journey to becoming a Nurse Practitioner. Information about accredited programs can typically be found on the websites of the CCNE and ACEN.
Understanding research principles is important for grasping evidence-based practice, a core tenet of accredited NP programs.
Certification and Licensure Process
After completing the rigorous educational requirements, the next steps for an aspiring Nurse Practitioner involve obtaining national certification and state licensure. These processes ensure that NPs meet established standards of competence and are legally authorized to practice.
National Certification Bodies
Upon graduating from an accredited Nurse Practitioner program, individuals must pass a national certification exam to become certified in their chosen specialty population focus. This certification demonstrates competency in a specific area of NP practice. The two main national certification bodies for NPs in the United States are the American Nurses Credentialing Center (ANCC) and the American Academy of Nurse Practitioners Certification Board (AANPCB), formerly AANPCP.
Both the ANCC and AANPCB offer various certification exams tailored to different NP roles and population foci, such as Family Nurse Practitioner (FNP), Adult-Gerontology Primary Care Nurse Practitioner (AGPCNP), Adult-Gerontology Acute Care Nurse Practitioner (AGACNP), Pediatric Nurse Practitioner (PNP), and Psychiatric-Mental Health Nurse Practitioner (PMHNP). The choice of certification exam depends on the NP's educational preparation and career goals. Passing one of these national exams is a critical step, as it is almost universally required for state licensure as an NP.
These certifying bodies establish eligibility criteria for their exams, which typically include holding an active RN license and graduating from an accredited NP program in the specialty area of the certification being sought. The exams themselves are competency-based and designed to assess the knowledge and skills required for safe and effective NP practice.
Preparing for these rigorous exams is a significant undertaking. Many resources are available to help NP graduates study, including review courses, practice tests, and study guides. Successfully passing a national certification exam signifies that an NP has met a national standard of excellence in their field.
Courses that focus on test preparation or offer broad reviews of medical topics can be helpful in this phase.
State-Specific Licensing Requirements
After achieving national certification, a Nurse Practitioner must obtain licensure in the state(s) where they intend to practice. Licensure is granted by the state's Board of Nursing (BON) and is a legal requirement to practice as an NP. While national certification demonstrates competency in a specialty, state licensure provides the legal authority to practice within that state's jurisdiction.
Licensing requirements vary from state to state, which can sometimes create challenges for NPs who wish to practice in multiple states or relocate. Generally, states require proof of graduation from an accredited NP program, current national certification in an appropriate specialty, and an active RN license. Some states may have additional requirements, such as specific coursework (e.g., in pharmacology or controlled substances prescribing), additional clinical hours beyond those required for certification, fingerprinting and background checks, or jurisprudence exams (testing knowledge of state nursing laws and regulations).
The scope of practice for NPs is also defined by state law and can differ significantly. Some states have "full practice authority," allowing NPs to practice independently to the full extent of their education and training. Other states have "reduced" or "restricted" practice, which may require NPs to have a collaborative agreement with a physician or limit their prescriptive authority. It is crucial for NPs to be thoroughly familiar with the Nurse Practice Act and associated regulations in any state where they are licensed or are seeking licensure.
Aspiring NPs should research the specific licensing requirements of their intended state(s) of practice early in their educational planning. Information can typically be found on the website of the respective state's Board of Nursing. OpenCourser offers resources like the Learner's Guide to help navigate such professional development steps.
Maintenance of Certification (CE Requirements)
Once certified and licensed, Nurse Practitioners must maintain their credentials through ongoing professional development, which typically includes completing a certain number of continuing education (CE) hours. Both national certification bodies (ANCC and AANPCB) and state Boards of Nursing have requirements for periodic renewal, usually every few to five years.
For national recertification, organizations like AANPCB require a minimum of 1,000 practice hours as an NP in the population focus of certification and at least 100 contact hours of advanced CE, with a specific portion (e.g., 25 hours) dedicated to advanced practice pharmacology, within the 5-year certification period. The ANCC has similar requirements, often involving 75 CE hours, with 25 in pharmacotherapeutics, plus fulfillment of other professional development categories like academic credits, presentations, research, or precepting. Precepting advanced healthcare students can sometimes be used to fulfill a portion of non-pharmacology CE credits.
State licensure renewal also typically requires CE, and these requirements may or may not align perfectly with national recertification mandates. For example, California requires RNs (including NPs) to complete 30 contact hours of CE every two years, with specific requirements for NPs working with geriatric populations. It is the NP's responsibility to track and fulfill all applicable CE requirements for both their national certification(s) and their state license(s). CE activities must generally be relevant to the NP's area of certification and practice and be approved by accredited providers.
Staying current with advancements in medicine, pharmacology, and patient care through continuing education is essential for providing high-quality care and maintaining professional competence throughout an NP's career.
Many online platforms offer CE courses suitable for NPs. OpenCourser can help you browse Health & Medicine courses to find relevant options.
Multistate Licensure Compact Details
For nurses, including Registered Nurses and Advanced Practice Registered Nurses (APRNs) like Nurse Practitioners, the ability to practice across state lines can be important for career flexibility and responding to healthcare needs in different areas. The Nurse Licensure Compact (NLC) and the APRN Compact are initiatives designed to facilitate this.
The NLC allows registered nurses (RNs) and licensed practical/vocational nurses (LPN/VNs) to have one multistate license, issued by their primary state of residence (home state), which authorizes them to practice in other NLC member states without needing to obtain separate licenses in each. This has been particularly beneficial for nurses who live near state borders, travel nurses, and for telehealth providers.
The APRN Compact aims to do something similar for APRNs, including Nurse Practitioners. If enacted by a sufficient number of states, it would allow an APRN who is licensed in a member state and meets the compact's uniform licensure requirements to practice in other member states, both physically and via telehealth. This is intended to improve access to care, especially in underserved areas and during public health emergencies, and to support APRN mobility. However, the adoption and implementation of the APRN Compact is an ongoing process, with different states at various stages of considering or enacting the necessary legislation. As of early 2024, several states had enacted the APRN Compact, but it was not yet operational as it requires a certain number of states to enact it before it can be implemented.
It's important for NPs to stay informed about the status of the APRN Compact in their state and in states where they might consider practicing. Information is typically available from the National Council of State Boards of Nursing (NCSBN), which has spearheaded these compact initiatives. Until the APRN Compact is widely adopted and implemented, NPs generally need to obtain individual state licenses for each state in which they wish to practice, a process that can be time-consuming and costly.
Career Progression and Specialization
A career as a Nurse Practitioner offers numerous avenues for growth, specialization, and advancement. From entry-level positions to senior and leadership roles, NPs can tailor their career paths to align with their interests and expertise, potentially moving into clinical leadership, academia, or research.
Entry-Level vs. Senior NP Roles
Upon completing their education and obtaining certification and licensure, new Nurse Practitioners typically enter entry-level roles. In these positions, they focus on applying their foundational knowledge and clinical skills, often managing a panel of patients under the guidance or collaboration of more experienced NPs or physicians, depending on state regulations and practice settings. Entry-level NPs concentrate on honing their diagnostic abilities, refining their treatment planning, and building confidence in managing a variety of health conditions within their specialty.
As NPs gain experience, often after several years in practice, they can progress to more senior roles. Senior NPs typically demonstrate a higher level of clinical expertise, autonomy, and leadership. They may take on more complex patient cases, mentor new NPs or nursing students, and contribute to quality improvement initiatives within their organizations. Senior NPs might also have greater responsibility in developing practice protocols, participating in research, or taking on administrative duties. Their advanced experience often allows them to serve as key resources for their colleagues and the broader healthcare team.
The transition from an entry-level to a senior NP role is a gradual process, marked by continuous learning, professional development, and the accumulation of clinical wisdom. This progression can also lead to increased earning potential and more diverse career opportunities.
Courses that build on foundational knowledge and introduce advanced concepts can support this progression.
Common Specialization Paths
Nurse Practitioners have the option to specialize in various areas of healthcare, allowing them to focus their expertise on specific patient populations or conditions. Choosing a specialization typically occurs during graduate education, as NP programs are geared towards preparing students for practice in a particular population focus. National certification is also specialty-specific.
Some of the most common NP specialization paths include:
- Family Nurse Practitioner (FNP): FNPs provide primary care to individuals and families across the lifespan, from infancy to old age. They are often the first point of contact for patients and manage a wide range of health issues. This is the largest specialty group among NPs.
- Adult-Gerontology Nurse Practitioner (AGNP): AGNPs specialize in the care of adults, including young adults, middle-aged adults, and older adults. They can focus on primary care (AG-PCNP) or acute care (AG-ACNP), managing both chronic and acute conditions in this population.
- Pediatric Nurse Practitioner (PNP): PNPs provide comprehensive healthcare to children, from birth through adolescence. They focus on growth and development, common childhood illnesses, and preventative care. Similar to AGNPs, they can specialize in primary care (PNP-PC) or acute care (PNP-AC).
- Psychiatric-Mental Health Nurse Practitioner (PMHNP): PMHNPs assess, diagnose, and treat individuals with mental health disorders and substance abuse issues. They provide therapy, manage psychotropic medications, and offer comprehensive mental health care.
- Women's Health Nurse Practitioner (WHNP): WHNPs focus on providing comprehensive reproductive and gynecological healthcare to women throughout their lives.
- Neonatal Nurse Practitioner (NNP): NNPs provide care to high-risk newborns, including premature infants and those with congenital conditions, typically in neonatal intensive care units (NICUs).
Beyond these primary population foci, NPs can further sub-specialize in areas like cardiology, dermatology, oncology, emergency medicine, orthopedics, or palliative care, often through on-the-job training, continuing education, and sometimes additional certifications. The choice of specialization often reflects an NP's passion and commitment to a particular area of patient care.
Exploring courses related to specific populations can help determine areas of interest.
Leadership Opportunities in Clinical Settings
Nurse Practitioners are increasingly recognized for their potential to take on leadership roles within clinical settings. Their advanced education, clinical expertise, and holistic approach to patient care position them well to influence healthcare delivery and improve patient outcomes. Leadership opportunities for NPs can range from formal management positions to informal roles as mentors and change agents.
Within hospitals, clinics, and other healthcare organizations, experienced NPs may advance to roles such as lead NP, clinical team leader, or department manager. In these positions, they might oversee other nursing staff, develop and implement clinical protocols, manage budgets, and contribute to strategic planning. NPs can also lead quality improvement projects, patient safety initiatives, and efforts to integrate evidence-based practices into care.
Beyond formal titles, NPs often demonstrate leadership through mentoring junior colleagues, precepting NP students, and advocating for their patients and the nursing profession. Many NPs are involved in professional organizations, where they can contribute to policy development, advocate for scope of practice advancements, and shape the future of nursing. The American Association of Nurse Practitioners (AANP) provides numerous avenues for NP leadership and advocacy. As healthcare systems continue to evolve, particularly with the shift towards value-based care, the leadership contributions of NPs are becoming even more critical.
For those with an inclination towards leadership, seeking out opportunities to take initiative, participate in committees, and further their education in healthcare management or administration can pave the way for impactful leadership roles. OpenCourser's Management category offers courses that can help develop these skills.
Courses focusing on healthcare management and policy can be particularly relevant for NPs aspiring to leadership.
Transitioning to Academic or Research Roles
For Nurse Practitioners with a passion for education or scientific inquiry, transitioning into academic or research roles offers another avenue for career development and impact. These paths allow NPs to contribute to the advancement of nursing knowledge, shape the next generation of nurses, and influence healthcare practices through evidence-based findings.
In academia, NPs can become faculty members in nursing schools and universities. Responsibilities often include teaching undergraduate and graduate nursing students, developing curriculum, mentoring students, and conducting scholarly work. Academic positions may require a doctoral degree, often a Doctor of Nursing Practice (DNP) for practice-focused faculty roles or a Doctor of Philosophy (PhD) in nursing for research-intensive faculty roles.
NPs interested in research can pursue careers as nurse researchers or scientists. This can involve designing and conducting clinical trials, analyzing health data, investigating the effectiveness of interventions, and disseminating findings through publications and presentations. Research roles may be found in academic institutions, healthcare systems, government agencies, or private industry. Similar to academic roles, advanced research positions often require a doctoral degree (DNP or PhD) and a strong foundation in research methodologies and statistical analysis. Some NPs may combine clinical practice with research or academic responsibilities, creating a hybrid role.
The transition to academia or research often involves further education, a commitment to scholarly activity, and the development of specialized skills in teaching or research. However, it offers the opportunity to make a broader impact on the nursing profession and patient care beyond direct clinical practice.
For those interested in research or academia, courses on research methodologies and educational principles are valuable.
Work Environments and Practice Settings
Nurse Practitioners are versatile healthcare professionals who can be found in a wide array of work environments. The setting in which an NP practices can influence their day-to-day responsibilities, patient populations, and overall work experience.
Hospital Systems vs. Private Practice Comparisons
Nurse Practitioners can find employment in large hospital systems or in smaller private practice settings, each offering distinct advantages and challenges. Hospital-based NPs often work in specialized units, emergency departments, or outpatient clinics affiliated with the hospital. Working within a large system typically provides access to a wide range of resources, advanced technology, and a diverse team of specialists for collaboration. Hospitals may also offer more structured career ladders, benefits packages, and opportunities for involvement in research or teaching.
In contrast, private practices, which can be physician-owned, NP-owned (in states with full practice authority), or group practices, often offer a more intimate setting. NPs in private practice may experience greater autonomy in their daily work and have more flexibility in scheduling and practice management, particularly if they are practice owners. They often build long-term relationships with a consistent panel of patients. However, private practices may have fewer administrative support staff and require NPs to take on more business-related responsibilities.
The choice between a hospital system and private practice often comes down to personal preference regarding work environment, level of autonomy desired, and career goals. Both settings offer opportunities for NPs to provide high-quality patient care and make a meaningful impact.
Telehealth Expansion Opportunities
Telehealth, the delivery of healthcare services remotely using telecommunications technology, has rapidly expanded in recent years, creating significant new opportunities for Nurse Practitioners. NPs are well-suited to provide care via telehealth due to their strong assessment, communication, and patient education skills. This mode of practice allows NPs to reach patients in new ways, improving access to care, especially for those in rural or underserved areas, or for individuals with mobility limitations.
NPs can utilize telehealth for a variety of services, including conducting routine check-ups, managing chronic conditions, providing mental health counseling, offering urgent care consultations, and prescribing medications (where legally permitted via telehealth). This can involve video conferencing, phone calls, and remote patient monitoring devices. The flexibility of telehealth can also offer NPs a different work-life balance, with some positions allowing for remote work.
While telehealth offers numerous benefits, it also presents challenges, such as ensuring patient privacy and data security, navigating varying state licensure and telehealth regulations, and adapting clinical assessment skills to a virtual environment. However, as technology continues to advance and patient acceptance of virtual care grows, telehealth is expected to remain a significant and expanding component of healthcare delivery, offering diverse career avenues for NPs. Many online courses in Health & Medicine now incorporate aspects of telehealth.
Courses focused on telehealth can equip NPs with the specific skills needed for this growing field.
Rural/Underserved Area Practice Incentives
Nurse Practitioners play a critical role in providing healthcare access to rural and underserved populations, areas often facing significant physician shortages. Recognizing this vital contribution, various incentives and programs exist to encourage NPs to practice in these communities. These incentives can help make practicing in high-need areas more attractive and financially viable.
Common incentives include loan repayment or forgiveness programs offered by federal and state governments, such as those administered by the National Health Service Corps (NHSC). These programs often require a commitment to practice for a certain number of years in a designated Health Professional Shortage Area (HPSA). Some states or local communities may also offer direct financial bonuses, relocation assistance, or housing support to attract NPs.
Practicing in a rural or underserved setting can be immensely rewarding, offering NPs the opportunity to make a profound impact on community health, often with a broader scope of practice and greater autonomy. However, it can also come with challenges, such as limited resources, professional isolation, and the need to manage a wide variety of complex health issues. Despite these challenges, many NPs find deep satisfaction in serving populations with the greatest need. Information about these opportunities and incentives can often be found through professional NP organizations, government health departments, and job boards specializing in rural healthcare.
Courses on population health and public health in crisis situations can provide relevant knowledge for working in these communities.
Academic Medical Center Roles
Academic Medical Centers (AMCs) offer unique and dynamic practice environments for Nurse Practitioners. These institutions combine patient care with medical education and research, creating a stimulating atmosphere for continuous learning and professional growth. NPs in AMCs often work as part of multidisciplinary teams, caring for patients with complex conditions and contributing to cutting-edge treatments and research.
In an AMC setting, NPs may have opportunities to be involved in teaching medical students, residents, and NP students, serving as preceptors or clinical faculty. They might also participate in clinical research studies, helping to advance medical knowledge and translate research findings into practice. The patient population in AMCs is often diverse and may include individuals with rare or complex diseases, providing NPs with exposure to a wide range of clinical challenges.
Working in an AMC can be demanding, often involving a fast-paced environment and a high acuity patient load. However, it also offers access to specialized resources, expert colleagues, and a culture of inquiry and innovation. For NPs who are passionate about lifelong learning, teaching, and being at the forefront of medical advancements, a career in an academic medical center can be exceptionally rewarding.
Books on the healthcare system and public health interventions offer valuable context for roles within complex organizations like AMCs.
Contemporary Challenges in NP Practice
Despite the significant contributions of Nurse Practitioners to healthcare, the profession faces ongoing challenges. These hurdles can impact an NP's daily practice, career progression, and the overall ability of the profession to meet the evolving healthcare needs of the population.
Scope-of-Practice Legislative Battles
One of the most significant ongoing challenges for Nurse Practitioners revolves around scope-of-practice laws. These are state-level regulations that define what services an NP is legally allowed to provide, including their ability to diagnose, treat, and prescribe medications independently. While many national organizations and studies support full practice authority for NPs – allowing them to utilize their full education and training without mandatory physician supervision or collaboration – the legislative landscape remains inconsistent across the United States.
As of early 2024, a number of states have adopted full practice authority, often leading to improved access to care, especially in underserved areas. However, in other states, NPs face restrictive or reduced practice environments, requiring career-long supervision or collaboration agreements with physicians, which can limit their autonomy and create barriers to care. These restrictions can also make it more challenging for NPs to establish their own practices or to bill for their services effectively.
The debate over NP scope of practice often involves physician groups who raise concerns about patient safety and the comparative extent of NP versus physician training. NP organizations, like the AANP, actively advocate for the removal of these barriers, citing extensive research demonstrating the safety and quality of NP care and the positive impact of full practice authority on healthcare access and costs. These legislative battles are ongoing and require continuous advocacy and engagement from the NP community to ensure that state laws reflect the capabilities and contributions of Nurse Practitioners.
Reimbursement Parity Issues
Reimbursement parity, or the equal payment for the same services regardless of who provides them, is another significant challenge for Nurse Practitioners. While NPs are authorized to provide many of the same services as physicians, particularly in primary care, they often receive lower reimbursement rates from Medicare, Medicaid, and private insurance companies for performing those identical services. For example, Medicare typically reimburses NPs at 85% of the physician fee schedule for the same service.
This disparity in reimbursement can have several negative consequences. It can disincentivize practices from hiring NPs or from utilizing them to their full potential. It can also create financial challenges for NP-owned practices, making it harder for them to remain viable, especially in underserved areas where reimbursement rates may already be lower. The lack of payment parity can be perceived as undervaluing the care provided by NPs, despite numerous studies demonstrating comparable patient outcomes and high patient satisfaction with NP care.
Advocacy efforts are underway by NP organizations to achieve fair and equitable reimbursement policies. The argument for parity is based on the principle of "equal pay for equal work" and the recognition that NPs provide high-quality, cost-effective care. Achieving reimbursement parity is seen as crucial for maximizing the NP workforce's potential to improve healthcare access and address provider shortages.
Understanding healthcare economics is important for grasping these reimbursement challenges.
Burnout and Workload Management
Like many healthcare professionals, Nurse Practitioners are susceptible to burnout, a state of emotional, physical, and mental exhaustion caused by prolonged or excessive stress. The demands of clinical practice, including heavy workloads, long hours, administrative burdens (such as electronic health record documentation), and the emotional toll of caring for sick patients, can contribute to NP burnout.
High patient volumes, insufficient staffing support, and challenges related to scope-of-practice restrictions or reimbursement can exacerbate workload pressures. Burnout can lead to decreased job satisfaction, increased risk of medical errors, and a higher likelihood of NPs leaving their positions or the profession altogether. This not only impacts the well-being of individual NPs but also has broader implications for patient care quality and workforce stability.
Strategies for preventing and mitigating burnout are crucial. These can include organizational initiatives such as optimizing staffing levels, streamlining administrative tasks, promoting a supportive work culture, and providing resources for mental health and wellness. Individual NPs can also employ self-care strategies, set healthy boundaries, seek peer support, and engage in stress-reducing activities. Effective workload management, including efficient scheduling and delegation of appropriate tasks, is also key. Recognizing the signs of burnout and addressing its root causes are important for sustaining a healthy and effective NP workforce.
Courses on stress management and self-care can be beneficial for all healthcare professionals, including NPs.
Reading about empathy in healthcare can also provide valuable perspectives.
Interprofessional Collaboration Barriers
While interprofessional collaboration is widely recognized as essential for optimal patient care, Nurse Practitioners can sometimes encounter barriers that hinder effective teamwork. These challenges can stem from various factors, including traditional hierarchical structures in healthcare, differing communication styles, lack of role clarity, and historical tensions between medical and nursing professions.
In some settings, there may be a lack of understanding or appreciation for the full scope of an NP's education, skills, and capabilities, leading to underutilization or a reluctance to fully integrate NPs into care teams. Differing philosophies of care or approaches to patient management can also create friction if not addressed through open communication and mutual respect. Furthermore, restrictive scope-of-practice laws that mandate physician supervision can sometimes create an imbalanced power dynamic rather than fostering a truly collaborative partnership.
Overcoming these barriers requires a commitment from all members of the healthcare team to foster a culture of collaboration, mutual respect, and shared decision-making. Strategies include promoting clear role delineation, establishing effective communication channels, encouraging joint training and education initiatives, and creating team-based care models that explicitly value the contributions of each profession. When NPs are empowered to work collaboratively and to the full extent of their abilities, it benefits not only the healthcare team but also, most importantly, the patients they serve.
Future Trends Impacting Nurse Practitioners
The healthcare landscape is constantly evolving, and several key trends are poised to significantly impact the Nurse Practitioner profession in the coming years. Staying abreast of these developments is crucial for NPs to adapt, thrive, and continue to meet the healthcare needs of the population effectively.
Projected Workforce Demands by Specialty
The demand for Nurse Practitioners is projected to grow significantly in the coming years. The U.S. Bureau of Labor Statistics (BLS) consistently ranks NP as one of the fastest-growing occupations. This growth is driven by several factors, including an aging population requiring more healthcare services, an increased emphasis on preventative care, and ongoing efforts to expand access to care, particularly in primary care and underserved areas.
Workforce demands are expected to vary by specialty. Given the national shortage of primary care providers, Family Nurse Practitioners (FNPs) and Adult-Gerontology Primary Care Nurse Practitioners (AG-PCNPs) are likely to remain in high demand. Additionally, with a growing focus on mental health, Psychiatric-Mental Health Nurse Practitioners (PMHNPs) are also a specialty with a strong and growing demand. As the population ages, NPs specializing in geriatrics and the management of chronic diseases will also be crucial.
Other specialty areas, such as acute care, pediatrics, and women's health, will continue to need qualified NPs. The BLS Occupational Outlook Handbook provides detailed projections and is a valuable resource for understanding future workforce needs. Aspiring and practicing NPs should consider these trends when making decisions about specialization and career development to align their skills with areas of greatest need and opportunity.
Technological Integration (AI in Diagnostics)
Technology is rapidly transforming healthcare delivery, and Nurse Practitioners will increasingly need to integrate new tools and systems into their practice. One of the most significant technological advancements is the rise of Artificial Intelligence (AI) in areas like diagnostics and clinical decision support. AI algorithms can analyze medical images, interpret lab results, identify patterns in patient data, and assist in formulating potential diagnoses or treatment options.
For NPs, AI has the potential to enhance diagnostic accuracy, improve efficiency, and personalize patient care. However, it also presents challenges. NPs will need to develop skills in using AI-powered tools effectively, understanding their capabilities and limitations, and critically evaluating their outputs. Ethical considerations, such as data privacy, algorithmic bias, and the impact on the clinician-patient relationship, will also need careful attention.
Beyond AI, other technologies like telehealth platforms, electronic health records (EHRs), remote patient monitoring devices, and mobile health apps are already integral to NP practice. Staying proficient with these technologies and adapting to new innovations will be essential for NPs to provide high-quality, contemporary care in the future. Continuous learning and professional development in health informatics and digital health will be increasingly important. You can find relevant courses by browsing Technology on OpenCourser.
Courses exploring the intersection of healthcare and technology can provide valuable insights.
Value-Based Care Model Implications
The healthcare system is gradually shifting from traditional fee-for-service models to value-based care models. Value-based care prioritizes the quality and outcomes of care over the sheer volume of services provided. This means that healthcare providers, including Nurse Practitioners, are increasingly being reimbursed based on their ability to improve patient health, enhance patient satisfaction, and reduce overall healthcare costs.
This shift has significant implications for NP practice. Nurse Practitioners, with their strong emphasis on health promotion, disease prevention, chronic disease management, and patient education, are well-positioned to excel in value-based care environments. Their holistic and patient-centered approach aligns well with the goals of improving outcomes and managing costs effectively.
In value-based models, NPs will likely play even more critical roles in care coordination, managing patient populations, and implementing strategies to prevent hospital readmissions and unnecessary emergency department visits. Skills in data analysis, quality improvement, and interprofessional teamwork will be highly valued. NPs will need to demonstrate the value they bring to patient care through measurable outcomes. This evolving payment landscape may also create new opportunities for NP-led practices that can effectively deliver high-quality, cost-efficient care.
Relevant books can shed light on the broader healthcare context.
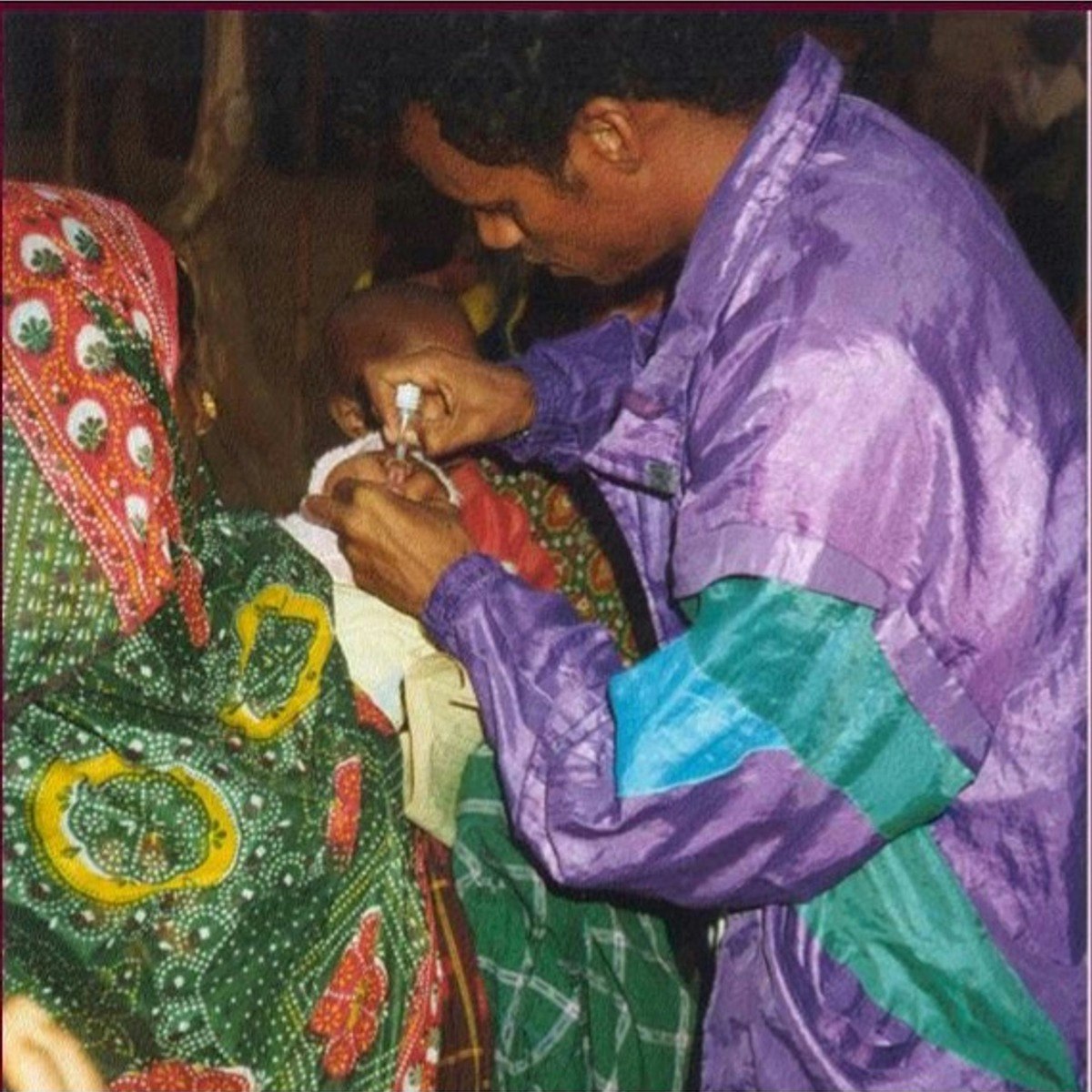
Global Health Initiatives Involving NPs
Nurse Practitioners are increasingly involved in global health initiatives, contributing their expertise to address health challenges in diverse international settings. As healthcare needs continue to grow worldwide, particularly in low- and middle-income countries, the skills and knowledge of NPs are highly valuable in strengthening health systems and improving access to care.
NPs may participate in global health through various avenues, including working with non-governmental organizations (NGOs), volunteering for short-term medical missions, participating in international research collaborations, or contributing to health education and training programs abroad. Their roles can involve providing direct patient care, training local healthcare workers, developing community health programs, and advocating for health policy changes.
The ability of NPs to provide a broad range of primary care services, manage chronic diseases, and focus on health promotion makes them particularly effective in resource-limited settings. Challenges in global health work can include navigating different cultural contexts, language barriers, limited resources, and complex ethical considerations. However, for NPs passionate about making a difference on a global scale, these opportunities offer profound personal and professional rewards. As the interconnectedness of global health becomes more apparent, the role of NPs in these initiatives is likely to expand.
Courses on public health and international health provide a good foundation for understanding global health challenges.
Frequently Asked Questions (Career Focus)
This section addresses common questions that individuals exploring a career as a Nurse Practitioner often have, focusing on practical considerations that can influence career decisions.
NP vs. PA Career Differences
Nurse Practitioners (NPs) and Physician Assistants (PAs) are both advanced practice providers who play crucial roles in healthcare, and their responsibilities can often overlap, leading to confusion about the differences. Both can diagnose illnesses, develop and manage treatment plans, and prescribe medications. However, their training philosophies, educational paths, and, in some cases, scopes of practice and practice autonomy differ.
NPs are trained under a nursing model, which typically emphasizes a holistic, patient-centered approach focusing on health promotion, disease prevention, and patient education. They begin as Registered Nurses, obtain a BSN, and then complete a graduate degree (MSN or DNP) focused on a specific patient population. NP practice autonomy varies by state, with some states allowing independent practice.
PAs, on the other hand, are educated in a medical model, which is similar to physician training and often focuses more on a disease-centered or biological systems approach. PA programs are typically master's level and require a bachelor's degree and specific science prerequisites, but not necessarily prior healthcare experience as an RN. PAs generally practice under the supervision of a physician, and their scope of practice is often determined by the supervising physician and state law. PAs often have more extensive training in specialized procedures and may have a greater role in pre-operative and post-operative care.
The choice between an NP and PA career often depends on an individual's preferred model of care, desired level of practice autonomy (which can be state-dependent for NPs), and educational background. Both professions offer rewarding opportunities to provide high-quality patient care. You can learn more about the Physician Assistant career path on OpenCourser.
Time Investment for Career Transition
Transitioning to a career as a Nurse Practitioner requires a significant time investment, particularly if starting without a nursing background. If you already hold a Bachelor of Science in Nursing (BSN) and are a Registered Nurse (RN), the path to becoming an NP typically involves completing a Master of Science in Nursing (MSN) program, which usually takes 18 months to 3 years, depending on whether you attend full-time or part-time. A Doctor of Nursing Practice (DNP) program, if pursued directly after a BSN, often takes 3 to 4 years of full-time study.
For individuals with an Associate Degree in Nursing (ADN) and RN licensure, an RN-to-BSN bridge program is typically required first, which can take about 2 years, followed by the MSN or DNP program. If you have a bachelor's degree in a field other than nursing, accelerated BSN programs (often 12-18 months) or direct-entry MSN programs (usually 3 years) are options to become an RN first, then pursue NP specialization within or after that program.
Beyond the formal education, time must also be allocated for clinical hours (hundreds to over a thousand, depending on the program and state), studying for and passing the national NP certification exam, and obtaining state licensure. Some NP programs may also require or prefer applicants to have one or more years of clinical experience as an RN before entry. Therefore, a career transition into an NP role can take anywhere from 2 to 7 years or more, depending on your starting point and the intensity of your studies. It’s a journey that demands dedication and careful planning, but for many, the rewards of an NP career make the investment worthwhile.
Loan Forgiveness Programs
The cost of graduate education to become a Nurse Practitioner can be substantial, leading many students to incur student loan debt. Fortunately, several loan forgiveness and repayment programs are available to help alleviate this financial burden, particularly for NPs willing to work in underserved communities or specific healthcare settings.
One of the most well-known federal programs is the National Health Service Corps (NHSC) Loan Repayment Program. This program offers significant loan repayment assistance to licensed primary care medical, dental, and mental and behavioral health providers, including NPs, who commit to working for at least two years at an NHSC-approved site in a Health Professional Shortage Area (HPSA). There is also an NHSC Scholarship Program that provides scholarships to students pursuing eligible health professions education in exchange for a service commitment in an underserved community.
Many states also have their own State Loan Repayment Programs (SLRPs), often funded in part by the federal government, which offer similar benefits for practice in designated shortage areas within that state. Additionally, some employers, particularly large healthcare systems or facilities in high-need areas, may offer loan repayment assistance as part of their benefits package. The Public Service Loan Forgiveness (PSLF) program is another federal option that may forgive the remaining balance on Direct Loans after 120 qualifying monthly payments have been made while working full-time for a qualifying employer (e.g., government or not-for-profit organizations).
Aspiring and practicing NPs should thoroughly research these programs, including eligibility criteria, service commitments, and application processes. Websites like the NHSC website and state health department websites are good starting points. Taking advantage of these programs can significantly reduce the financial stress of NP education.
Part-Time Practice Feasibility
For Nurse Practitioners seeking flexibility in their careers, part-time practice is often a feasible option. Many healthcare settings, including clinics, hospitals, and private practices, offer part-time positions for NPs. This can be an attractive choice for NPs who are balancing work with family responsibilities, pursuing further education, phasing into retirement, or simply desiring a better work-life balance.
The availability of part-time NP roles can vary by geographic location, specialty, and the overall demand for NPs in a particular area. In some high-demand specialties or underserved regions, finding part-time work may be easier. Telehealth has also expanded opportunities for flexible and part-time NP work, as some positions may allow for remote patient care on a part-time basis.
It's important for NPs considering part-time work to understand how it might affect benefits (such as health insurance or retirement contributions), salary (which is typically prorated), and opportunities for career advancement. Maintaining licensure and certification, including fulfilling continuing education and practice hour requirements, is still necessary even when working part-time. Networking, utilizing professional NP organizations, and working with healthcare recruiters can be helpful strategies for finding part-time NP positions.
International Practice Opportunities
For Nurse Practitioners interested in working abroad, international practice opportunities do exist, though navigating the requirements can be complex. The recognition of the NP role and the scope of practice for NPs vary significantly from country to country. Some countries have well-established NP roles similar to those in the United States, while in others, the concept of an advanced practice nurse may be less developed or not formally recognized.
To practice as an NP in another country, individuals will typically need to meet that country's specific education, licensure, and registration requirements. This might involve having credentials evaluated, passing local examinations, demonstrating language proficiency, and obtaining work visas. The process can be lengthy and require extensive research and preparation. Professional nursing organizations in the target country or international nursing councils can often provide information on the requirements.
Alternatively, NPs may find international opportunities through volunteer organizations, non-governmental organizations (NGOs) involved in global health, or with multinational corporations that employ healthcare providers for their international staff. The U.S. military also employs NPs who may be stationed abroad. While challenging, international practice can offer NPs unique experiences to broaden their clinical skills, learn about different healthcare systems, and contribute to global health efforts.
Malpractice Insurance Considerations
Like all healthcare providers who diagnose and treat patients, Nurse Practitioners need to have professional liability insurance, commonly known as malpractice insurance. This insurance provides coverage in the event that an NP is named in a malpractice lawsuit alleging negligence or harm to a patient resulting from their professional services.
The cost and type of malpractice insurance an NP needs can vary based on several factors, including their specialty, practice setting (e.g., hospital vs. private practice), geographic location (some states have higher malpractice rates), employment status (employed vs. self-employed/independent contractor), and the scope of services they provide. NPs who are employed by hospitals or large clinics are often covered under their employer's group malpractice policy. However, it's crucial for employed NPs to understand the extent of this coverage and whether they might need their own supplemental policy.
NPs who own their own practices or work as independent contractors are responsible for obtaining their own malpractice insurance. There are two main types of malpractice policies: "claims-made" policies, which cover claims reported while the policy is active (and may require purchasing "tail" coverage if the NP leaves the practice or retires), and "occurrence" policies, which cover any incident that occurred during the policy period, regardless of when the claim is filed. Understanding the differences and choosing the right policy is essential. Several insurance companies specialize in providing malpractice coverage for healthcare professionals, including NPs.
Conclusion
The journey to becoming a Nurse Practitioner is one of dedication, rigorous education, and a commitment to lifelong learning and patient advocacy. It is a career path that offers immense personal and professional rewards, providing the opportunity to make a profound difference in the lives of individuals, families, and communities. NPs are at the forefront of healthcare, blending clinical expertise with a compassionate, holistic approach to care. They are leaders, educators, researchers, and, above all, trusted healthcare providers. As the healthcare landscape continues to evolve, the role of the Nurse Practitioner will only become more vital. For those with the ambition and passion to pursue this challenging yet fulfilling career, the path, while demanding, leads to a profession that is not only in high demand but also deeply impactful. Whether you are just starting to explore this option or are well on your way, resources like OpenCourser can help you find the online courses and information you need to navigate your educational and career journey. The path to becoming an NP is an investment in a future where you can truly shape the health and well-being of others.
If you are considering a career in healthcare, OpenCourser offers a vast library of courses to explore. You can browse thousands of courses across various disciplines. For those looking to save on their educational journey, be sure to check out the deals page for the latest offers on online courses and learning resources.