Sports Medicine Physician
A Career Guide to Becoming a Sports Medicine Physician
Sports medicine represents a specialized area of healthcare focused on the physical fitness, injury prevention, and treatment of athletes and active individuals. A sports medicine physician is a medical doctor who has completed extensive training in diagnosing and managing conditions related to physical activity. They work not just with professional athletes, but also with children, adolescents, adults engaged in recreational sports, and even individuals with physically demanding jobs.
What makes this field particularly engaging is the blend of medical science with the dynamic world of sports and physical activity. Sports medicine physicians often work closely with patients who are highly motivated to recover and return to their passions. This career path allows physicians to apply their medical knowledge in diverse settings, from clinics and hospitals to the sidelines of sporting events, contributing directly to the health and performance of active people.
Furthermore, the field is constantly evolving with advancements in diagnostic tools, treatments, and rehabilitation techniques. This ensures a stimulating environment where continuous learning is essential. For those passionate about both medicine and physical activity, becoming a sports medicine physician offers a unique and rewarding way to combine these interests.
What Does a Sports Medicine Physician Do?
Diagnosing and Treating Sports-Related Injuries
A core responsibility of a sports medicine physician is the accurate diagnosis of injuries sustained during sports or physical activity. This involves taking detailed patient histories, performing thorough physical examinations, and often interpreting imaging studies like X-rays, MRI scans, or diagnostic ultrasounds. Common conditions treated include sprains, strains, fractures, dislocations, tendonitis, and overuse injuries.
Once a diagnosis is made, the physician develops a tailored treatment plan. Importantly, most sports injuries (estimated around 90%) do not require surgery. Therefore, sports medicine physicians excel in non-operative management, utilizing methods such as medication, injections, bracing, and coordinating care with other specialists. Their goal is to restore function and alleviate pain effectively.
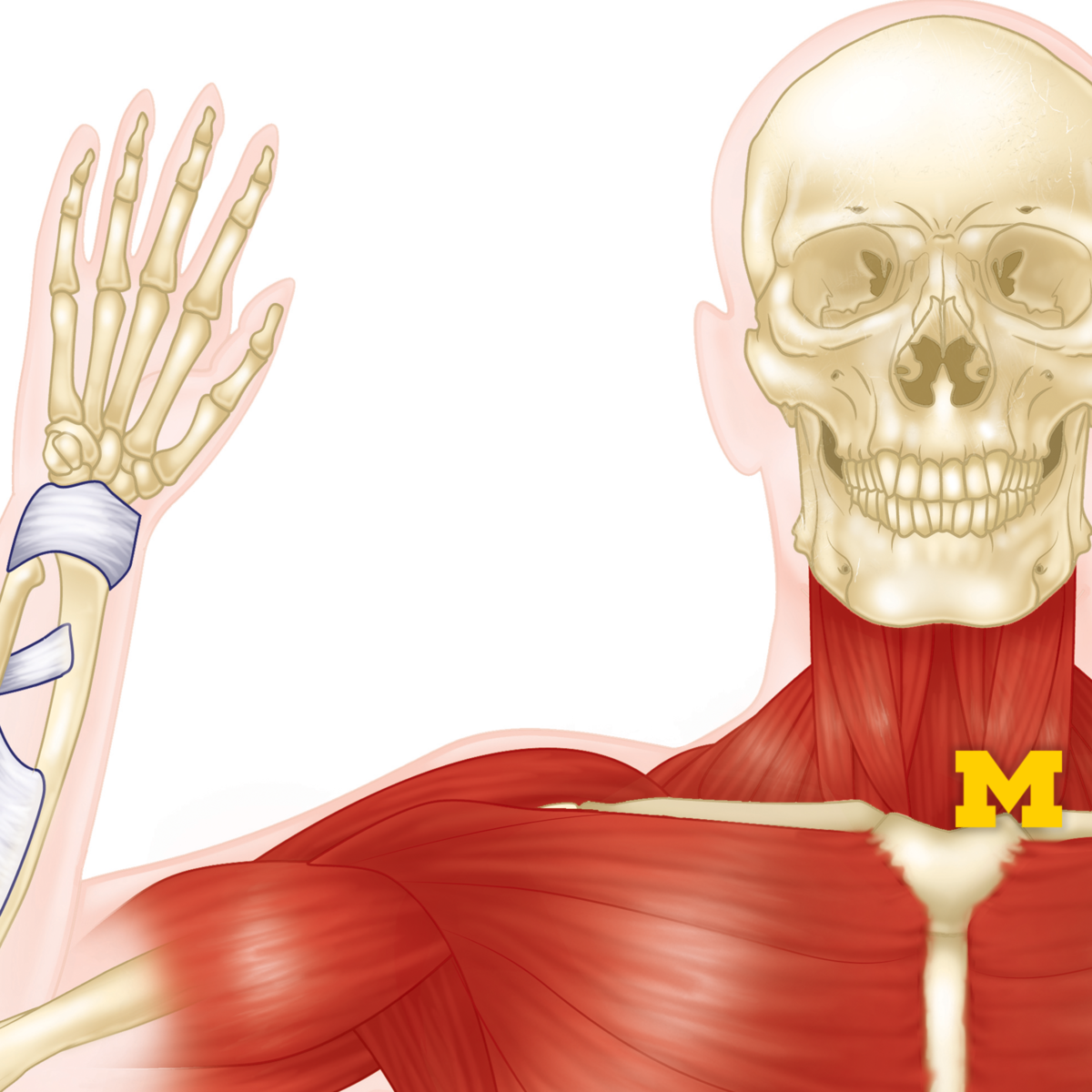
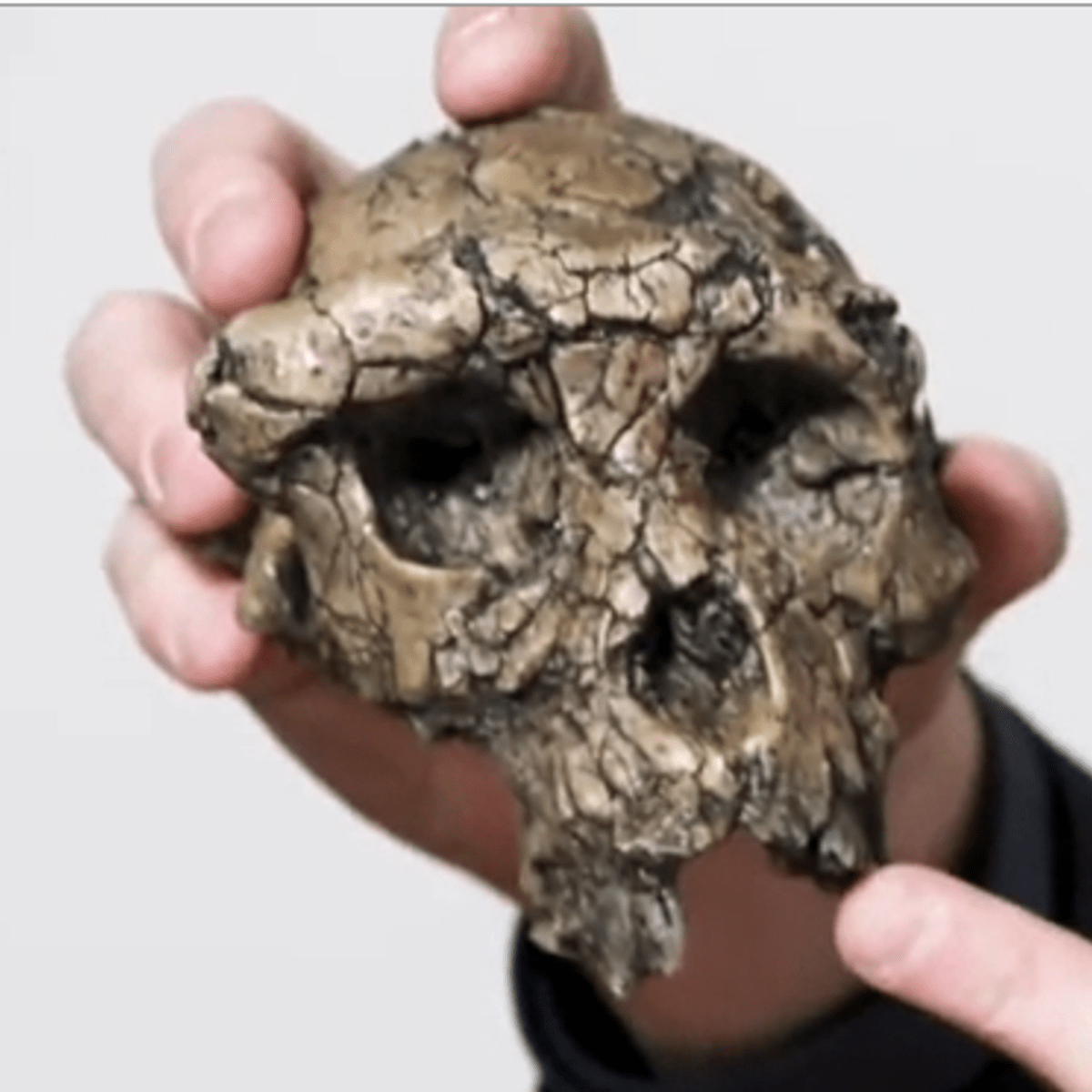
Understanding the intricacies of the musculoskeletal system is fundamental. These courses provide foundational knowledge relevant to diagnosing and managing common sports injuries.
Developing Rehabilitation and Injury Prevention Strategies
Treatment often extends beyond immediate care into rehabilitation. Sports medicine physicians design and oversee rehab programs, frequently collaborating with physical therapists, to help patients regain strength, flexibility, and endurance. The focus is not just recovery, but returning the individual safely to their desired activity level, minimizing the risk of re-injury.
Proactive injury prevention is another critical aspect of the role. Physicians educate patients, coaches, and parents on proper techniques, conditioning principles, appropriate equipment use, and recognizing early warning signs of injury. They may also conduct pre-participation physical examinations (PPEs) to identify potential risk factors before an athlete starts a season.
These resources offer insights into preventing injuries, a key component of sports medicine practice, and understanding how the body adapts to physical demands.
These books delve deeper into rehabilitation techniques and the comprehensive management of sports injuries.
Collaboration and Team-Based Care
Sports medicine is inherently collaborative. Physicians work closely with a network of professionals, including athletic trainers, physical therapists, orthopedic surgeons (when surgery is needed), coaches, nutritionists, and exercise physiologists. Effective communication and teamwork are essential to provide comprehensive care tailored to the individual's needs and goals.
In team settings, the sports medicine physician often serves as the lead medical contact, coordinating care, making return-to-play decisions, and ensuring athlete health and safety protocols are followed. This involves liaising between the athlete, coaching staff, and other healthcare providers, ensuring everyone is informed and aligned on the plan of care.
This collaborative spirit fosters a holistic approach, addressing not only the physical injury but also factors like nutrition, conditioning, and even the psychological aspects of recovery and performance. Such teamwork is vital for optimizing outcomes for active individuals.
Expanding Roles Beyond Athletes
While often associated with elite athletes, the expertise of sports medicine physicians benefits a much broader population. They treat "weekend warriors," young athletes, and adults engaging in fitness programs. Their knowledge of musculoskeletal injuries and non-surgical treatments is applicable to anyone leading an active life.
Furthermore, their understanding of biomechanics and ergonomics can be applied in occupational health settings. They might advise on preventing workplace injuries related to physical tasks or help manage musculoskeletal conditions aggravated by job duties. This demonstrates the versatility of the specialty.
The principles of exercise prescription and promoting healthy lifestyles are also central to their practice. They advise individuals on safe ways to start or maintain physical activity, helping manage chronic conditions like arthritis or diabetes through exercise, aligning with initiatives like Exercise is Medicine®, a global health initiative managed by the American College of Sports Medicine (ACSM).
The Long Road: Educational Pathways
Undergraduate Foundation and Pre-Medical Studies
The journey begins with a four-year bachelor's degree. While medical schools don't mandate a specific major, common choices include biology, chemistry, physics, or dedicated pre-medicine tracks. What's crucial is completing the prerequisite coursework, typically heavy in sciences like biology, general chemistry, organic chemistry, physics, and mathematics, alongside humanities and social sciences.
Beyond coursework, aspiring physicians need strong academic performance (GPA) and a competitive score on the Medical College Admission Test (MCAT). Extracurricular activities demonstrating leadership, teamwork, community service, and clinical exposure (like volunteering or shadowing physicians) are also vital components of a strong medical school application.
This undergraduate phase is rigorous and demands discipline and commitment. It lays the scientific and personal foundation necessary for the challenges of medical training. It's also a time for self-reflection to ensure medicine is the right path.
Medical School: MD or DO
Following undergrad, the next step is four years of medical school, leading to either a Doctor of Medicine (MD) or Doctor of Osteopathic Medicine (DO) degree. Both degrees qualify graduates to practice medicine in all specialties, including sports medicine. DO programs include additional training in osteopathic manipulative medicine (OMM), a hands-on diagnostic and therapeutic approach.
The first two years typically focus on foundational sciences – anatomy, physiology, biochemistry, pathology, pharmacology – and introductions to clinical skills and medical ethics. The final two years consist of clinical rotations, where students gain hands-on experience in various hospital and clinic settings, working directly with patients under supervision across different medical specialties.
Medical school is an intense period of learning, requiring significant dedication and resilience. It builds the core knowledge and clinical skills essential for any physician, regardless of their eventual specialty.
This comprehensive book provides an essential overview of human anatomy, critical for all medical training.
Residency Training: The Primary Specialty
After medical school, graduates enter residency training. Importantly, sports medicine itself is not a primary residency specialty in the United States. Instead, physicians first complete a residency in a different field, typically lasting three to five years. Common residency pathways for future sports medicine physicians include Family Medicine, Pediatrics, Internal Medicine, Emergency Medicine, or Physical Medicine and Rehabilitation (PM&R).
Each of these residencies provides a strong foundation in general medical care or a specific patient population, which is essential before specializing further. For instance, a Family Medicine residency offers broad training across ages and conditions, while Pediatrics focuses on children and adolescents. Orthopedic Surgery is another pathway, but it leads to surgical sports medicine, distinct from primary care sports medicine.
Residency is a demanding period involving long hours and significant responsibility, where physicians refine their clinical skills, diagnostic reasoning, and patient management abilities under the guidance of experienced attendings. It is during this time that crucial practical experience is gained.
Fellowship: Specializing in Sports Medicine
Following successful completion of a primary residency, physicians interested in non-surgical sports medicine pursue a fellowship. This is typically a one-to-two-year program dedicated specifically to sports medicine training. It's during the fellowship that physicians deepen their expertise in musculoskeletal injury diagnosis and management, concussion care, sports performance, and related medical issues in active populations.
Fellowship training involves extensive clinical work in sports medicine clinics, time spent with orthopedic surgeons (including observing surgeries to better understand indications and post-operative care), and significant hands-on experience as a team physician for high school, collegiate, or sometimes professional sports teams. Fellows learn to manage injuries on the sidelines, in the training room, and in clinical settings.
This specialized training builds upon the foundation laid during residency, equipping physicians with the specific knowledge and skills required to practice sports medicine effectively. Completion of an accredited fellowship is necessary to become eligible for board certification in sports medicine.
Licensing and Board Certification
To practice medicine independently, all physicians must obtain a state medical license. This requires graduating from an accredited medical school, completing residency training, and passing a national licensing examination series (the USMLE for MDs or the COMLEX-USA for DOs).
After residency, physicians typically become board-certified in their primary specialty (e.g., Family Medicine, Pediatrics). Following fellowship, they can then sit for the Certificate of Added Qualifications (CAQ) in Sports Medicine examination, administered jointly by several primary specialty boards. Passing this exam signifies board certification in sports medicine.
Board certification demonstrates a high level of expertise and commitment to the specialty. Maintaining certification requires ongoing continuing medical education (CME) and periodic re-certification exams (typically every 10 years), ensuring physicians stay current with the latest advancements in the field throughout their careers.
Leveraging Online and Continuing Education
The Role of Online Courses in Skill Development
While formal medical education and training are irreplaceable, online courses offer valuable supplementary learning opportunities. They can help build foundational knowledge in related areas or provide deeper dives into specific topics relevant to sports medicine. Platforms like OpenCourser aggregate thousands of courses, making it easier to find relevant content.
For aspiring physicians or those early in training, online courses in anatomy, physiology, biomechanics, or exercise science can reinforce concepts learned in formal schooling. For practicing physicians, online modules offer convenient ways to earn Continuing Medical Education (CME) credits required for maintaining licensure and board certification.
Online learning provides flexibility, allowing learners to study at their own pace and on their own schedule. This is particularly beneficial for busy students and professionals seeking to expand their knowledge base without disrupting clinical responsibilities. Many courses offer certificates upon completion, which can be added to a CV or professional profile.
Discover a wide range of courses in health and medicine through OpenCourser's dedicated category page.
Health & Medicine Courses on OpenCourser
Key Topics for Self-Study and Enrichment
Beyond core medical training, several areas are particularly beneficial for sports medicine physicians to explore through self-study or continuing education. Understanding biomechanics, the science of movement, is crucial for analyzing injury mechanisms and optimizing performance. Nutrition plays a significant role in athlete health, recovery, and performance, making courses or readings in sports nutrition highly relevant.
Topics like exercise physiology delve into how the body responds and adapts to physical stress. Familiarity with strength and conditioning principles helps in advising patients on training programs. Additionally, understanding the psychological aspects of injury, recovery, and competition can enhance patient care.
Online platforms offer courses covering these diverse subjects, allowing individuals to tailor their learning to specific interests or knowledge gaps. Engaging with these topics demonstrates a commitment to comprehensive patient care within the sports medicine context.
These courses explore movement, training principles, and nutrition, all vital components of sports medicine knowledge.
This book offers comprehensive insights into sports nutrition, a critical aspect of athlete care.
Certifications for Specialized Techniques
Sports medicine involves various procedures and specialized techniques. Continuing education often includes hands-on workshops or certification courses for skills like musculoskeletal ultrasound. Ultrasound is increasingly used for diagnosing injuries and guiding injections accurately in the clinic setting.
Other specialized certifications might relate to specific manual therapy techniques, concussion assessment tools, or emergency procedures relevant to sideline coverage. While not always mandatory, these certifications can enhance a physician's skillset and marketability.
Professional organizations like the American Medical Society for Sports Medicine (AMSSM) and the American College of Sports Medicine (ACSM) often host or endorse such training opportunities, frequently available through conferences or dedicated courses, some of which may have online components.
These courses offer introductions to specific manual techniques sometimes used adjunctively in musculoskeletal care, though formal certification typically requires in-person training.
Integrating Online Learning with Clinical Practice
The true value of online learning lies in its application to real-world clinical practice. Knowledge gained from courses on new diagnostic approaches, treatment modalities, or rehabilitation protocols can directly inform patient care decisions. Staying updated through online resources helps physicians provide evidence-based care.
Online platforms can also facilitate case discussions or provide access to expert lectures, fostering a community of learning. Physicians can use online databases and journals accessed through platforms or institutional subscriptions to research specific patient cases or stay abreast of the latest research findings.
Ultimately, continuous learning, whether through formal CME, online courses, or self-directed study, is integral to being an effective sports medicine physician. It ensures that practitioners remain competent, adaptable, and capable of providing the highest standard of care in a dynamic field.
Charting Your Course: Career Progression and Opportunities
Entry-Level Roles and Initial Steps
The formal entry into the specialized practice of sports medicine begins with the fellowship. During this 1-2 year period, physicians gain intensive, focused experience under supervision. They work in clinics, training rooms, and on the sidelines, managing a wide range of sports-related conditions and learning the practical aspects of team physician coverage.
Upon completing the fellowship and obtaining board certification in sports medicine, physicians typically seek their first attending positions. Early roles might be in academic medical centers, large hospital systems, multi-specialty groups, or private orthopedic practices. Some may combine sports medicine duties with their primary specialty (e.g., seeing family medicine patients part-time).
Initial years focus on building clinical experience, refining procedural skills (like injections or ultrasound), establishing referral networks, and possibly continuing team coverage responsibilities started during fellowship, perhaps at the high school or small college level.
Mid-Career Opportunities and Advancement
With several years of experience, sports medicine physicians often find diverse opportunities for growth. Many build thriving clinical practices within hospital systems or private groups, becoming known experts in their community. Some may take on roles with progressively higher levels of responsibility in team coverage, potentially working with major university athletic departments or professional sports teams.
Mid-career physicians might also develop niche interests, focusing on specific populations (like pediatric athletes) or conditions (like concussion management). Leadership opportunities can arise within their practice group, hospital department, or professional organizations. Teaching medical students, residents, or fellows is another common avenue for experienced physicians, particularly in academic settings.
Compensation generally increases with experience and practice maturity. According to Salary.com data from early 2025, the average annual salary for a sports medicine physician in the US is around $292,755, with typical ranges between $263,624 and $312,242. However, salaries can vary significantly based on location, experience, practice setting (academic vs. private), and primary specialty background.
Leadership and Academic Pathways
For those inclined towards leadership or academia, several paths exist. Within a clinical practice or hospital system, experienced physicians might become medical directors of sports medicine programs or clinics. Serving on committees or in leadership roles within professional societies like AMSSM or ACSM offers opportunities to influence the field nationally.
In academic medicine, physicians progress through faculty ranks (Assistant, Associate, Full Professor). This typically involves a combination of clinical care, teaching trainees, and conducting research. Academic roles often provide opportunities to lead fellowship programs, contribute to scientific literature, and shape the future generation of sports medicine physicians.
These leadership and academic roles require not only clinical expertise but also strong communication, mentoring, administrative, and often research skills. They offer a way to have a broader impact on the field beyond individual patient care.
Entrepreneurial Ventures and Consulting
Some sports medicine physicians pursue entrepreneurial paths. This could involve establishing their own private practice or specialized sports medicine clinic. This route offers autonomy but also requires business acumen in addition to clinical skills, managing aspects like staffing, billing, and marketing.
Consulting opportunities may also arise. Physicians might consult for sports equipment companies on product design and safety, advise organizations on health and wellness programs, or provide expertise for sports technology startups. Others may engage in medicolegal consulting, providing expert opinions for legal cases involving sports injuries.
These paths often appeal to physicians seeking greater independence or wishing to leverage their expertise in non-traditional ways. Success requires initiative, networking, and often, additional business or specialized knowledge.
Building the Foundation: Essential Skills and Competencies
Mastering Clinical Skills
Strong clinical skills form the bedrock of sports medicine practice. This includes proficiency in taking detailed patient histories focused on activity levels and injury mechanisms. Performing comprehensive musculoskeletal examinations to accurately identify pathology is paramount. Interpreting diagnostic imaging, such as X-rays, MRIs, and musculoskeletal ultrasound, is also crucial.
Physicians must be adept at various non-surgical treatment techniques. This includes appropriate medication management, joint and soft tissue injections (often guided by ultrasound), application of braces or casts, and prescribing effective rehabilitation programs. Procedural skills require ongoing practice and refinement.
Excellent diagnostic reasoning is essential to differentiate between various conditions presenting with similar symptoms. This involves integrating information from the history, physical exam, and diagnostic tests to arrive at an accurate diagnosis and formulate an effective management plan.
These courses enhance understanding of human movement and anatomy, crucial for clinical assessment.
These comprehensive texts are staples in sports medicine, covering clinical practice and surgical techniques often relevant even for non-surgeons to understand.
Communication and Patient Education
Effective communication is vital in sports medicine. Physicians must clearly explain complex medical conditions and treatment plans to patients, families, coaches, and other members of the care team in understandable language. Building rapport and trust is essential, especially when working with athletes under pressure.
Patient education is a key component of care. This involves teaching patients about their injury, the recovery process, strategies for preventing recurrence, and the importance of adhering to rehabilitation protocols. Empowering patients with knowledge helps improve compliance and outcomes.
Strong interpersonal skills are needed to navigate potentially sensitive conversations, such as discussing return-to-play limitations, managing expectations about recovery timelines, or addressing the psychological impact of injuries. Empathy and active listening are crucial attributes.
Knowledge of Sports Science and Nutrition
A solid understanding of exercise physiology, biomechanics, and sports nutrition differentiates sports medicine physicians. This knowledge helps in understanding injury mechanisms, designing effective rehabilitation and conditioning programs, and advising on performance optimization.
Knowing how different types of training affect the body allows physicians to provide informed guidance on safe progression and injury prevention. Understanding nutritional requirements for athletes helps in advising on diet for optimal performance, recovery, and overall health.
This scientific foundation allows physicians to address the athlete holistically, considering factors beyond just the immediate injury. It enables them to provide comprehensive care that supports both health and performance goals.
These courses and books cover training principles and nutrition specifically for athletic populations.
Adaptability and Technological Fluency
The field of sports medicine is constantly evolving with new research, diagnostic tools, and treatment techniques. Physicians must be lifelong learners, committed to staying updated through continuing education, reading medical literature, and attending conferences. Adaptability is key to incorporating new evidence-based practices.
Technological fluency is increasingly important. This includes proficiency with electronic health record (EHR) systems, interpreting advanced imaging, and understanding the role of emerging technologies like wearable sensors for monitoring athletes or telemedicine for remote consultations. Familiarity with tools like diagnostic ultrasound is becoming standard.
Embracing innovation allows physicians to provide state-of-the-art care. This might involve learning new injection techniques, utilizing regenerative medicine approaches where appropriate, or incorporating data analytics into practice.
Where You'll Work: Environments and Specializations
Clinical Settings vs. Field-Side Roles
Sports medicine physicians work in various settings. Many practice primarily in outpatient clinics, either within hospital systems, multi-specialty groups, or private orthopedic practices. In this setting, they see scheduled patients for diagnosis, treatment, and follow-up of musculoskeletal conditions.
A distinct aspect of the field is the opportunity for field-side or training room coverage. This involves working directly with sports teams, providing immediate care during practices and competitions. This role requires quick decision-making under pressure, managing acute injuries, and making return-to-play judgments on the spot.
Many physicians blend these roles, spending part of their week in the clinic and dedicating other times to team coverage. The balance depends on the specific job and the physician's interests. Field-side roles often involve irregular hours, including evenings and weekends, and potential travel with the team.
Subspecialties and Niche Areas
Within sports medicine, physicians can develop further subspecialty interests. Pediatric sports medicine focuses specifically on the unique injuries and developmental considerations of young athletes. Concussion management is another major area, requiring specialized knowledge in diagnosis, treatment, and safe return-to-play protocols.
Some physicians focus on specific types of athletes (e.g., runners, dancers) or particular joints (e.g., shoulder, knee). Others may specialize in procedures like musculoskeletal ultrasound or regenerative medicine techniques like Platelet-Rich Plasma (PRP) therapy. This specialization often develops through experience and targeted continuing education.
Developing a niche can enhance a physician's expertise and reputation, potentially leading to referrals and unique career opportunities. It allows for deeper engagement with a specific area of interest within the broader field.
Research and Academic Opportunities
For those interested in advancing the field, research and academic positions offer rewarding pathways. Academic sports medicine physicians typically work at universities or teaching hospitals, combining clinical practice with teaching medical students, residents, and fellows.
Research opportunities involve investigating injury mechanisms, evaluating new treatments, studying injury prevention strategies, or exploring physiological responses to exercise. This can range from clinical trials to epidemiological studies or laboratory-based research. Publishing findings in peer-reviewed journals and presenting at conferences are key aspects of academic life.
An academic career allows physicians to contribute to the evidence base that guides clinical practice and to train the next generation of sports medicine professionals. It requires strong analytical skills, a commitment to scholarly activity, and often, additional research training.
Global Demand and Regional Variations
The demand for sports medicine expertise exists globally, driven by increasing participation in sports and recreational activities across all age groups. However, the structure of practice, specific job opportunities, and compensation can vary significantly by country and region.
In the United States, the field is well-established with defined training pathways and board certification. Opportunities exist in diverse settings, though the job market can be competitive, particularly for positions with high-profile teams or in desirable locations. Some sources suggest the market is quite saturated, especially for those seeking 100% sports medicine roles right out of fellowship.
Internationally, the role and recognition of sports medicine physicians might differ. Opportunities may exist with national sports federations, Olympic committees, or within different healthcare system structures. Understanding the local context is crucial for those considering practice outside their home country.
Consider exploring related careers which often collaborate closely with sports medicine physicians.
Navigating the Field: Ethical and Safety Considerations
Balancing Athlete Health and Competitive Pressures
A significant ethical challenge in sports medicine is navigating the inherent tension between an athlete's long-term health and the short-term pressures to compete and win. Coaches, teams, and sometimes athletes themselves may push for a premature return to play after an injury.
The physician's primary ethical obligation is to the patient's well-being. This requires making objective medical decisions based on the athlete's readiness and safety, even if it conflicts with competitive goals. Clear communication about risks and benefits, and advocating for the athlete's health, are crucial.
This challenge is particularly acute when working as a team physician, where loyalties might feel divided. Maintaining professional boundaries and adhering to ethical guidelines is paramount in these high-pressure situations.
Doping and Performance Enhancement Controversies
Sports medicine physicians play a role in educating athletes about anti-doping rules and the health risks associated with performance-enhancing substances. They must be knowledgeable about prohibited substances lists maintained by organizations like the World Anti-Doping Agency (WADA).
Ethical dilemmas can arise if physicians are pressured to prescribe substances for performance enhancement or overlook potential doping activities. Adherence to strict ethical codes and anti-doping regulations is non-negotiable. Physicians may also be involved in therapeutic use exemptions (TUEs), where an athlete requires a prohibited substance for a legitimate medical condition.
Promoting fair play and athlete health requires a firm stance against doping and a commitment to ethical prescribing practices. Understanding the nuances of sports pharmacology and anti-doping protocols is essential.
These books explore the complex ethical issues surrounding doping in sports.
Informed Consent and Novel Treatments
As sports medicine evolves, new and sometimes experimental treatments emerge, such as certain regenerative medicine therapies. Physicians have an ethical responsibility to ensure patients fully understand the risks, benefits, alternatives, and evidence (or lack thereof) supporting such treatments before proceeding.
Obtaining truly informed consent requires clear communication, avoiding overly optimistic claims, and ensuring the patient comprehends the information, especially when dealing with novel or off-label therapies. Financial conflicts of interest related to specific treatments must also be disclosed.
Maintaining scientific rigor and prioritizing patient safety over the allure of cutting-edge but unproven therapies is a key ethical responsibility. Decisions should always be guided by the best available evidence and the patient's specific circumstances and values.
Mental Health Advocacy for Athletes
There is growing recognition of the importance of mental health in sports. Athletes face unique pressures related to performance, injury, public scrutiny, and balancing their sport with other life demands. Sports medicine physicians are often well-positioned to identify signs of mental health issues like depression, anxiety, or eating disorders.
While not typically primary mental health providers, sports medicine physicians have a role in screening for mental health concerns, providing initial support, and referring athletes to appropriate mental health professionals when needed. Creating a supportive environment where athletes feel comfortable discussing mental health is crucial.
Advocating for the integration of mental health services within sports organizations and destigmatizing mental health issues are important aspects of holistic athlete care. Recognizing the bidirectional relationship between physical and mental health is key to optimizing overall well-being and performance.
Keeping Pace: Industry Trends Impacting the Field
Advances in Regenerative Medicine
Regenerative medicine is a rapidly advancing area with significant potential in sports medicine. Techniques like Platelet-Rich Plasma (PRP) therapy and stem cell therapy aim to enhance the body's natural healing processes for injuries to tendons, ligaments, muscles, and joints. These approaches hope to accelerate recovery and improve tissue repair quality.
While research is ongoing and clinical applications are still evolving, these therapies represent a major trend. Sports medicine physicians need to stay informed about the latest evidence regarding the efficacy, safety, and appropriate indications for these treatments to guide patients effectively.
The appeal of potentially faster recovery times makes regenerative medicine a focal point of interest for athletes and physicians alike, driving further research and innovation in the field.
Telemedicine and Remote Patient Monitoring
The adoption of telemedicine has accelerated, significantly impacting sports medicine delivery. Remote consultations allow physicians to connect with athletes regardless of location, providing expert advice, follow-up care, and initial assessments conveniently. This is particularly useful for athletes traveling or those in areas with limited access to specialists.
Wearable technology enables remote monitoring of athletes' physiological data, training loads, and recovery metrics. Physicians can use this data to track progress, adjust treatment plans remotely, and potentially identify early signs of overtraining or injury risk, allowing for proactive interventions.
These technologies enhance accessibility to care, facilitate continuous monitoring, and offer new ways to manage athlete health and performance, representing a significant shift in how sports medicine can be practiced.
These resources delve into the latest trends shaping the future of sports medicine.
Growing Focus on Youth and Amateur Athlete Care
While elite athletes often capture headlines, there's a growing emphasis on providing high-quality sports medicine care to youth and amateur athletes. Increased participation rates in youth sports have highlighted the need for specialized care addressing growth-related injuries, concussion management in younger populations, and injury prevention education for parents and coaches.
This trend creates opportunities for sports medicine physicians in community settings, schools, and youth sports organizations. Addressing the specific needs of developing athletes requires knowledge of pediatric musculoskeletal development and age-appropriate treatment strategies.
The focus extends to promoting safe participation and long-term health for recreational adult athletes as well, recognizing that the benefits of physical activity apply across the lifespan, but injuries can occur at any level.
This course specifically addresses the science behind training young athletes safely and effectively.
Impact of AI and Data Analytics
Artificial intelligence (AI) and data analytics are beginning to influence sports medicine. AI algorithms can analyze large datasets from wearable sensors, electronic health records, and imaging studies to identify injury risk patterns, predict recovery trajectories, or assist in diagnostic interpretation.
Data analytics helps optimize training loads, monitor athlete readiness, and personalize prevention strategies based on individual biomechanics or physiological responses. This data-driven approach aims to make athlete management more precise and proactive.
While still an emerging area, the potential for AI to enhance diagnostic accuracy, personalize treatment plans, and improve injury prediction suggests it will become an increasingly important tool for sports medicine physicians in the future.
Facing the Hurdles: Challenges in Sports Medicine
High-Pressure Decision-Making
Working in competitive sports environments often involves making critical decisions under intense pressure. Determining an athlete's fitness to play during a crucial game, managing acute injuries on the sidelines with limited resources, and balancing health risks against performance demands require confidence and sound clinical judgment.
The visibility of these decisions, especially when working with high-profile teams or athletes, adds another layer of stress. Media scrutiny and expectations from fans, coaches, and team management can weigh heavily on physicians.
This high-stakes environment demands resilience, excellent communication skills, and the ability to remain objective and prioritize athlete safety even amidst external pressures.
Managing Chronic vs. Acute Injuries
Sports medicine physicians manage both sudden, acute injuries (like fractures or ligament tears) and chronic, overuse conditions (like tendonitis or stress fractures). Chronic injuries can be particularly challenging, often requiring prolonged treatment, activity modification, and careful management of athlete expectations regarding recovery timelines.
Distinguishing between different types of injuries, understanding the underlying biomechanical factors contributing to overuse conditions, and developing long-term management plans require deep clinical expertise. Helping athletes navigate the frustration of chronic conditions is also part of the role.
Successfully managing this spectrum of injuries necessitates a versatile skill set and a patient-centered approach tailored to the specific nature of the condition and the individual's goals.
These books address the specific challenges of running injuries and the broader epidemiology of sports injuries.
Work-Life Balance in Team-Based Roles
While rewarding, roles involving team coverage can significantly impact work-life balance. Games and practices often occur during evenings and weekends, requiring physicians to be present outside typical clinic hours. Travel with teams for away games or tournaments adds further time commitment.
Team physicians are often expected to be available 24/7 for urgent issues concerning their athletes. This constant availability, combined with the irregular schedule, can be demanding and potentially lead to burnout if not managed carefully.
Achieving a sustainable work-life balance often requires setting clear boundaries, effective time management, and strong support systems both professionally and personally. It's a significant consideration for those drawn to the allure of working directly with sports teams.
Navigating Regulatory and Healthcare System Changes
Like all medical fields, sports medicine is subject to evolving healthcare regulations, insurance policies, and documentation requirements. Staying compliant with these changes requires ongoing administrative effort and can impact practice efficiency.
Changes in reimbursement models, prior authorization requirements for treatments or imaging, and evolving guidelines for specific conditions (like concussion protocols mandated by sports governing bodies) add complexity to clinical practice.
Physicians must remain adaptable and informed about the broader healthcare landscape to navigate these systemic challenges effectively while continuing to provide high-quality patient care.
Frequently Asked Questions (FAQs)
Is sports medicine only for professional athletes?
No, definitely not. While sports medicine physicians are well-known for working with elite athletes, they treat a wide range of active individuals. This includes children involved in school sports, recreational adult athletes ("weekend warriors"), individuals starting new exercise programs, and even people with physically demanding jobs who suffer musculoskeletal injuries. Their expertise benefits anyone seeking to maintain an active lifestyle safely.
How competitive is the job market?
The job market for sports medicine physicians can be competitive, particularly for highly desirable positions like those with professional or major collegiate teams, or roles in popular geographic locations. Completing a fellowship is essential, but even then, securing a position that is 100% focused on sports medicine immediately after training can be challenging. Some sources suggest the market has become more saturated in recent years, and networking or connections made during training can be important. Flexibility in job scope (e.g., combining sports medicine with primary care) or location may increase opportunities. The overall outlook for physicians, according to the U.S. Bureau of Labor Statistics, projects growth roughly average for all occupations, but competition within specific subspecialties like sports medicine exists.
Can I transition from general practice to sports medicine?
Yes, transitioning is possible, but it typically requires additional formal training. The standard pathway involves completing a primary care residency (like Family Medicine, Internal Medicine, Pediatrics, or Emergency Medicine) and then applying for and completing a 1-2 year sports medicine fellowship program. This fellowship provides the specialized training necessary to practice sports medicine and become board-certified in the subspecialty. Direct transition without fellowship training is generally not the standard route to becoming a recognized sports medicine specialist.
What is the salary range at different career stages?
Salaries vary based on experience, location, practice setting (academic vs. private), and primary specialty background. Entry-level sports medicine physicians (just out of fellowship) might earn slightly less than the average. Salary.com reported an average annual salary around $292,755 in the US as of early 2025, with senior-level physicians potentially earning over $300,000. ZipRecruiter data from March 2025 showed an average of $217,445, with a range from $190,000 (25th percentile) to $244,500 (75th percentile). Experienced physicians, especially those in private practice or working with high-profile teams, may earn significantly more. Academic positions often pay less than private practice.
Are there opportunities for international work?
Yes, opportunities for sports medicine physicians exist internationally. This could involve working with national sports governing bodies, Olympic committees, international sports teams, or within different healthcare systems abroad. However, medical licensing requirements, recognition of credentials, practice scope, and compensation structures vary significantly between countries. Physicians interested in working internationally would need to thoroughly research the specific requirements and opportunities in their target country.
How does sports medicine differ from physical therapy or orthopedic surgery?
These are distinct but related fields. Sports Medicine Physicians (Primary Care) are medical doctors who complete a primary care residency followed by a sports medicine fellowship; they specialize in non-surgical treatment of musculoskeletal injuries and medical conditions related to sports and exercise. Orthopedic Surgeons are medical doctors who complete a residency in orthopedic surgery; they treat musculoskeletal conditions, often through surgery, though they also manage non-operative cases. Some orthopedic surgeons complete further fellowship training in surgical sports medicine. Physical Therapists are healthcare professionals (typically with a Doctor of Physical Therapy, DPT degree) who specialize in rehabilitation, helping patients recover strength, mobility, and function after injury through exercise and manual therapy, often working closely with physicians.
Choosing a career as a Sports Medicine Physician is a commitment to a long and rigorous path of education and training. It demands a passion for both medicine and physical activity, strong clinical skills, excellent communication abilities, and a dedication to lifelong learning. While challenging, it offers the unique reward of helping active individuals recover from injuries, prevent future problems, optimize their performance, and maintain healthy lifestyles. If you are drawn to the dynamic intersection of healthcare and the world of sports and exercise, this demanding yet fulfilling career may be an excellent path to explore.