Cardiovascular Disease
vigating the Landscape of Cardiovascular Disease: A Comprehensive Guide
Cardiovascular disease (CVD) encompasses a range of conditions that affect the heart and blood vessels. These diseases represent a significant global health challenge, being the leading cause of death worldwide. Understanding the intricacies of CVD, from its basic mechanisms to the latest treatment innovations and career opportunities, is crucial for anyone considering a path in this dynamic field. This article aims to provide a comprehensive overview, helping you determine if a journey into the world of cardiovascular health aligns with your aspirations.
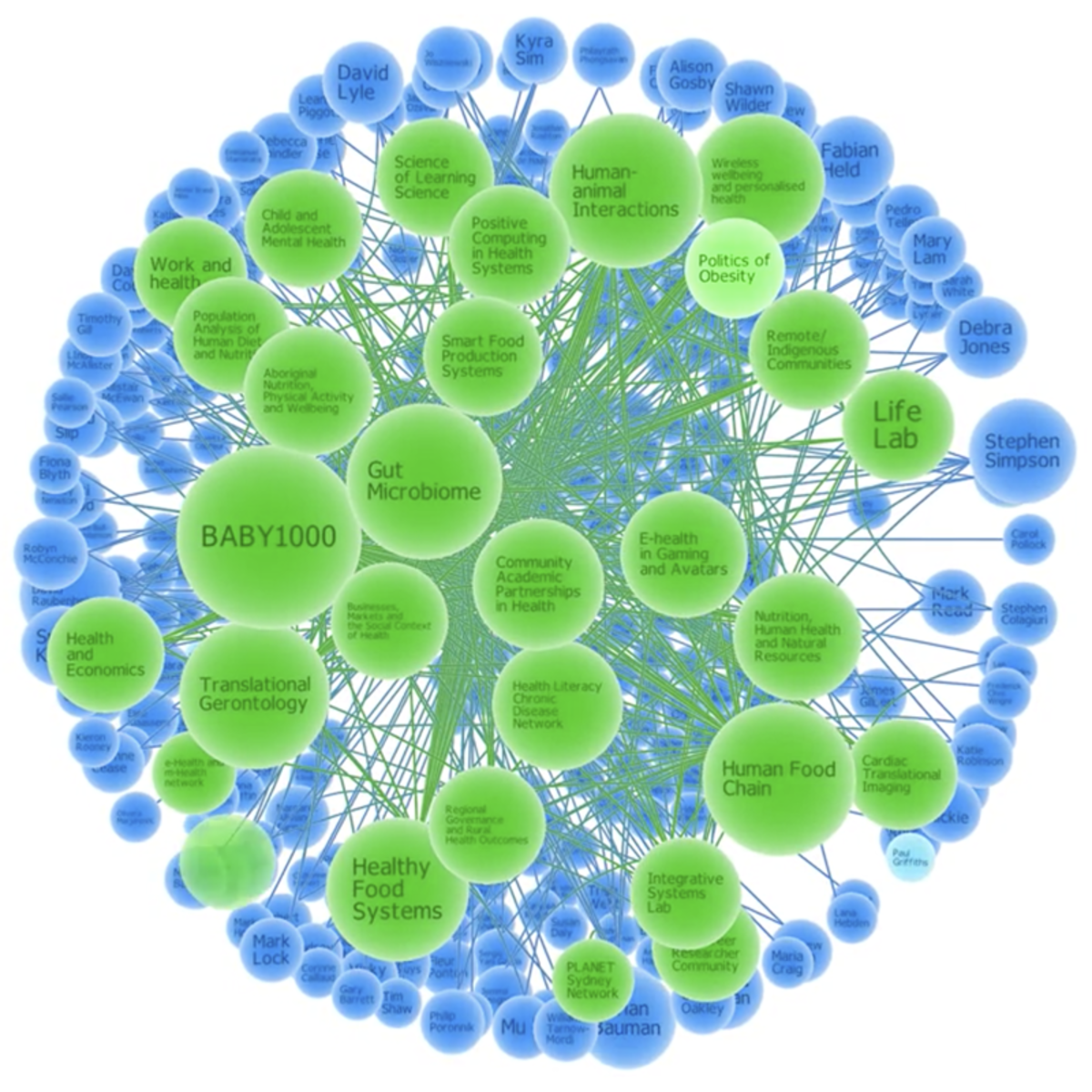
Working in the field of cardiovascular disease offers numerous engaging and exciting aspects. Professionals in this area are at the forefront of medical advancements, constantly seeking new ways to diagnose, treat, and prevent heart and blood vessel conditions. The interdisciplinary nature of the field means collaboration with a diverse range of experts, from molecular biologists to public health officials, fostering a rich learning environment. Furthermore, the direct impact on patient lives, improving health outcomes and quality of life, provides a profound sense of purpose and fulfillment for those dedicated to combating this global health issue.
Introduction to Cardiovascular Disease
Understanding cardiovascular disease is the first step toward exploring a career or further study in this critical area of health. This section will lay the groundwork by defining CVD, exploring its worldwide impact, briefly touching on its historical context, and outlining its significant societal and economic consequences.
Definition and Scope of Cardiovascular Disease (CVD)
Cardiovascular disease (CVD) is an umbrella term for a variety of disorders that affect the heart and blood vessels. These conditions can involve the heart muscle itself, the valves within the heart, the rhythm of the heartbeat, or the blood vessels throughout the body. Essentially, any disease process that impairs the normal functioning of the cardiovascular system falls under this broad category. The scope of CVD is vast, ranging from conditions present at birth (congenital heart disease) to those that develop over a lifetime due to lifestyle factors and other underlying health issues.
The major types of CVD include coronary artery disease (CAD), which affects the blood vessels supplying the heart muscle; cerebrovascular disease, which impacts the blood vessels supplying the brain and can lead to stroke; peripheral arterial disease, affecting blood vessels in the arms and legs; and rheumatic heart disease, resulting from damage to heart valves due to rheumatic fever. Other significant conditions include heart failure, where the heart cannot pump blood effectively, and arrhythmias, which are irregular heartbeats. Understanding these distinctions is crucial as each type of CVD has unique causes, mechanisms, and treatment approaches.
The complexity of CVD lies not only in its varied forms but also in the interconnectedness of the cardiovascular system. A problem in one area can often lead to complications in others. For instance, uncontrolled high blood pressure (hypertension) can strain the heart and blood vessels, increasing the risk of heart attacks, strokes, and heart failure over time. Similarly, the buildup of fatty deposits in arteries, known as atherosclerosis, is a common underlying factor in many forms of CVD, restricting blood flow and potentially leading to serious events.
Global Prevalence and Mortality Statistics
Cardiovascular diseases are the leading cause of death globally, claiming an estimated 17.9 million lives each year. This staggering figure represents approximately 32% of all global deaths. Of these CVD-related deaths, a significant majority, about 85%, are due to heart attacks and strokes. These statistics underscore the immense public health challenge posed by CVD worldwide.
The burden of cardiovascular disease is not evenly distributed. Over three-quarters of CVD deaths occur in low- and middle-income countries. Furthermore, a substantial portion of these deaths are premature, occurring in individuals under the age of 70. This highlights the urgent need for effective prevention and treatment strategies, particularly in resource-limited settings. The rising global death toll from CVD is largely attributed to growing and aging populations, although death rates have declined in many countries due to improved prevention and treatment.
In the United States alone, heart disease is the leading cause of death for men, women, and people of most racial and ethnic groups. Approximately one person dies every 33 seconds from cardiovascular disease in the U.S. These statistics not only represent a significant loss of life but also place a considerable strain on healthcare systems and economies. Early detection and management are critical in mitigating the devastating impact of CVD.
Brief Historical Context of CVD Research and Treatment
The understanding and treatment of cardiovascular disease have evolved dramatically over centuries. Early observations of the heart and circulatory system laid the groundwork, but significant advancements in diagnosis and treatment began to accelerate in the 20th century. The invention of the electrocardiogram (ECG) in the early 1900s provided the first non-invasive tool to study the heart's electrical activity, revolutionizing cardiac diagnostics.
The mid-20th century saw landmark epidemiological studies, such as the Framingham Heart Study, which began in 1948. This ongoing research identified major risk factors for cardiovascular disease, including high blood pressure, high cholesterol, smoking, obesity, and diabetes. This knowledge paved the way for preventive strategies. Simultaneously, surgical interventions like open-heart surgery and coronary artery bypass grafting emerged, offering new hope for patients with severe heart conditions.
Later decades brought further breakthroughs, including the development of cardiac catheterization techniques for diagnosis and treatment (like angioplasty and stenting), advanced cardiac imaging modalities, and a wide array of effective medications such as statins, beta-blockers, and ACE inhibitors. More recently, research has focused on genetic predispositions, molecular pathways, and the role of inflammation in CVD, leading to more targeted therapies and personalized medicine approaches. The journey of CVD research and treatment is a testament to continuous scientific inquiry and innovation, transforming what was once an almost invariably fatal set of conditions into manageable, and often preventable, diseases.
Key Societal and Economic Impacts
The societal and economic impacts of cardiovascular disease are profound and far-reaching. Beyond the immeasurable human cost of premature death and disability, CVD places a significant burden on healthcare systems, economies, and communities worldwide. Healthcare expenditures related to CVD are substantial, encompassing costs for hospital care, medications, diagnostic procedures, and long-term management. In the United States, heart disease costs were estimated at about $252.2 billion from 2019 to 2020, including healthcare services, medicines, and lost productivity due to death.
Lost productivity is another major economic consequence. Individuals suffering from CVD may be unable to work or may have reduced work capacity, leading to decreased income for families and lower economic output for nations. Premature deaths from CVD also result in a significant loss of potential years of productive life. The ripple effects extend to families who may face financial hardship due to medical expenses and the loss of a primary earner. Furthermore, the need for informal caregiving by family members can also impact their own employment and economic well-being.
From a societal perspective, the high prevalence of CVD can strain social support systems and impact overall quality of life within communities. The burden of disease can disproportionately affect vulnerable populations, exacerbating health inequities. However, investments in prevention, early detection, and effective treatment of CVD can yield significant returns, not only in terms of improved health outcomes but also in reduced healthcare costs and increased economic productivity. Public health initiatives and policies that promote heart-healthy lifestyles play a crucial role in mitigating these societal and economic impacts.
Types and Mechanisms of Cardiovascular Disease
Delving deeper into cardiovascular disease requires an understanding of its various forms and the intricate biological processes that drive them. This section is tailored for those with a foundational knowledge of biology and medicine, such as university students, researchers, and practitioners. We will explore common types of CVD, their underlying pathophysiology, genetic and molecular influences, and the crucial roles of inflammation and metabolic dysfunction.
Coronary Artery Disease, Heart Failure, Stroke, and Arrhythmias
Among the most prevalent and impactful cardiovascular diseases are coronary artery disease (CAD), heart failure, stroke, and arrhythmias. Each represents a distinct challenge to the cardiovascular system. Coronary Artery Disease (CAD), also known as coronary heart disease, is the most common type of heart disease. It occurs when the coronary arteries, which supply oxygen-rich blood to the heart muscle, become narrowed or blocked, typically due to the buildup of plaque (atherosclerosis). This reduced blood flow can lead to chest pain (angina) and, if a blockage is severe or sudden, a heart attack (myocardial infarction).
Heart Failure does not mean the heart has stopped working, but rather that it isn't pumping blood as well as it should to meet the body's needs. This can result from conditions that damage or weaken the heart, such as CAD, high blood pressure, or previous heart attacks. Symptoms often include shortness of breath, fatigue, and swelling in the legs and feet. Heart failure can affect the heart's ability to pump effectively (systolic dysfunction) or its ability to fill with blood properly (diastolic dysfunction).
Stroke occurs when the blood supply to part of the brain is interrupted or severely reduced, depriving brain tissue of oxygen and nutrients, which can cause brain cells to die within minutes. Strokes are primarily categorized as ischemic (caused by a blockage in an artery) or hemorrhagic (caused by a leaking or bursting blood vessel). Cerebrovascular disease is the underlying condition affecting the blood vessels supplying the brain. Finally, Arrhythmias are abnormal heart rhythms. They occur when the electrical impulses that coordinate heartbeats don't work properly, causing the heart to beat too fast (tachycardia), too slow (bradycardia), or irregularly. Some arrhythmias are harmless, while others can be life-threatening, increasing the risk of stroke or sudden cardiac arrest.
To deepen your understanding of these critical conditions, the following course provides a global perspective on non-communicable diseases, including cardiovascular disease.
Pathophysiology: Atherosclerosis, Hypertension, Thrombosis
The development of many cardiovascular diseases is rooted in specific pathophysiological processes, with atherosclerosis, hypertension, and thrombosis playing central roles. Atherosclerosis is a chronic inflammatory condition characterized by the buildup of fatty deposits, cholesterol, cellular waste products, calcium, and fibrin in the inner lining of an artery. This buildup, known as plaque, can progressively narrow the artery, restricting blood flow. If a plaque ruptures, it can trigger the formation of a blood clot that can completely block the artery, leading to events like a heart attack or stroke.
Hypertension, or high blood pressure, is a condition where the force of blood against the artery walls is consistently too high. Over time, uncontrolled hypertension can damage arteries, making them less elastic and more prone to narrowing. It also forces the heart to work harder to pump blood, which can lead to an enlarged heart (hypertrophy) and eventually heart failure. Hypertension is a major risk factor for atherosclerosis, stroke, heart attack, and kidney disease.
Thrombosis refers to the formation of a blood clot (thrombus) inside a blood vessel, obstructing the flow of blood through the circulatory system. While blood clotting is a normal and essential process to stop bleeding after an injury, inappropriate clot formation within an artery or vein can have serious consequences. Arterial thrombosis is often a complication of atherosclerosis, where a ruptured plaque triggers clot formation. Venous thrombosis, such as deep vein thrombosis (DVT), occurs in veins and can lead to a pulmonary embolism if the clot breaks off and travels to the lungs. These three processes are often interconnected and contribute significantly to the burden of CVD.
For those looking to explore the multifaceted nature of chronic diseases and their interconnections, this course offers valuable insights.
This Spanish-language course provides an in-depth look at cardiovascular disease, focusing on risk assessment, diagnosis, and treatment plans for prevalent conditions.
Genetic and Molecular Contributors
While lifestyle factors play a significant role, genetic and molecular factors also make substantial contributions to the development of cardiovascular disease. Family history is a well-recognized risk factor, suggesting an inherited predisposition for certain conditions. Researchers have identified numerous genes associated with an increased risk of CVD, influencing factors like cholesterol metabolism, blood pressure regulation, blood clotting, and the inflammatory response. For example, familial hypercholesterolemia is a genetic disorder characterized by very high levels of low-density lipoprotein (LDL) cholesterol, leading to premature atherosclerosis and an increased risk of heart attacks.
At the molecular level, intricate signaling pathways and cellular processes are involved in the initiation and progression of CVD. Endothelial dysfunction, the impaired ability of the inner lining of blood vessels to function normally, is an early event in atherosclerosis. This involves reduced production of nitric oxide, a molecule crucial for vasodilation and inhibiting platelet aggregation and inflammation. Molecular mediators like cytokines, growth factors, and adhesion molecules orchestrate the inflammatory response within the vessel wall, contributing to plaque formation and instability.
Understanding these genetic and molecular underpinnings is crucial for developing targeted therapies and personalized approaches to CVD prevention and treatment. Advances in genomics and molecular biology continue to uncover new insights into the complex interplay of genes and environment in cardiovascular health. For instance, research into microRNAs and other non-coding RNAs is revealing their roles in regulating gene expression related to cardiac function and disease. These discoveries hold promise for novel diagnostic markers and therapeutic interventions.
Role of Inflammation and Metabolic Dysfunction
Inflammation and metabolic dysfunction are increasingly recognized as critical drivers in the development and progression of cardiovascular disease. While inflammation is a natural defense mechanism, chronic, low-grade inflammation plays a central role in atherosclerosis, from the initial stages of plaque formation to the eventual rupture of unstable plaques that can trigger heart attacks or strokes. Inflammatory cells, such as macrophages, infiltrate the arterial wall, releasing cytokines and enzymes that contribute to plaque growth and instability.
Metabolic dysfunction, encompassing conditions like obesity, insulin resistance, and type 2 diabetes (often collectively referred to as metabolic syndrome), creates a pro-inflammatory and pro-atherogenic environment. Insulin resistance, a key feature of metabolic syndrome, impairs the body's ability to use insulin effectively, leading to elevated blood glucose levels. This state is associated with endothelial dysfunction, abnormal lipid profiles (high triglycerides and low HDL cholesterol), and increased production of inflammatory markers, all of which accelerate atherosclerosis. Central obesity, characterized by excess abdominal fat, is particularly linked to chronic inflammation, as adipose tissue can release pro-inflammatory substances.
The interplay between inflammation and metabolic dysfunction creates a vicious cycle that significantly elevates CVD risk. For example, inflammatory mediators can worsen insulin resistance, while metabolic abnormalities can fuel further inflammation. Recognizing these connections has led to new therapeutic strategies aimed at reducing inflammation and correcting metabolic imbalances to prevent or treat cardiovascular disease. Lifestyle modifications, such as a healthy diet and regular physical activity, are crucial in addressing both inflammation and metabolic dysfunction.
The following course explores the concept of the exposome and how environmental factors, including those influencing metabolic health and inflammation, contribute to disease.
Formal Education Pathways in Cardiovascular Health
Pursuing a career dedicated to cardiovascular health typically involves a structured and rigorous educational journey. Whether your ambition is to become a clinician, a researcher, or a public health professional specializing in CVD, understanding the formal education pathways is essential. This section outlines the typical academic routes, from undergraduate prerequisites to specialized doctoral and clinical training, highlighting the interdisciplinary nature of this field.
For those considering this path, remember that dedication and perseverance are key. The years of study are demanding, but the potential to make a significant impact on human health is immense. If you are passionate about science and helping others, exploring these educational avenues could be the first step toward a deeply rewarding career.
Undergraduate Prerequisites (Biology, Chemistry)
A strong foundation in the basic sciences is essential for anyone aspiring to a career in cardiovascular health. Typically, undergraduate programs that serve as a launchpad for medical school, graduate research, or other health professions will require a core curriculum heavily focused on biology and chemistry. Courses in general biology will introduce fundamental concepts such as cell biology, genetics, physiology, and evolution, all of which are critical for understanding the complexities of the human body and disease processes like CVD.
Chemistry is equally vital. General chemistry courses cover atomic structure, bonding, reactions, and thermodynamics, providing the building blocks for understanding biochemical processes. Organic chemistry, which focuses on carbon-containing compounds, is particularly important as it forms the basis for understanding the structure and function of biological molecules, including proteins, lipids, and nucleic acids, as well as the mechanisms of drug action. Many programs also recommend or require courses in physics, which helps in understanding biomechanics and the physical principles underlying diagnostic technologies, and mathematics, including calculus and statistics, which are crucial for research and data analysis.
Beyond these core science courses, aspiring cardiovascular health professionals may benefit from coursework in areas like biochemistry, molecular biology, anatomy, and physiology to gain a more specialized understanding relevant to the cardiovascular system. Excelling in these prerequisite courses not only ensures eligibility for advanced programs but also develops the critical thinking and problem-solving skills necessary for a successful career in this challenging and rewarding field. Many medical schools also look for a well-rounded education, so humanities and social science courses can also be valuable.
Graduate Programs: Cardiology, Public Health, Biomedical Research
Following an undergraduate degree, several graduate-level pathways can lead to a career focused on cardiovascular health. For those aspiring to become medical doctors specializing in heart conditions, the path involves medical school followed by a residency in internal medicine and then a specialized fellowship in Cardiology. This extensive training, typically lasting a minimum of 10 years post-undergraduate, equips physicians with the clinical skills to diagnose, treat, and manage a wide range of cardiovascular diseases.
A Master's or Doctoral degree in Public Health (MPH or DrPH) offers a different but equally vital route. Public health professionals with a focus on cardiovascular disease work on prevention, epidemiology, health policy, and community health programs. They analyze population-level data to identify risk factors, design interventions to promote heart-healthy behaviors, and advocate for policies that support cardiovascular health. Their work is crucial in addressing the societal and environmental determinants of CVD.
For individuals passionate about discovery and innovation, graduate programs in Biomedical Research (M.S. or Ph.D.) provide the training to conduct scientific investigations into the fundamental mechanisms of cardiovascular disease, develop new diagnostic tools, or pioneer novel therapies. These research-intensive programs often focus on areas like molecular biology, genetics, pharmacology, or bioengineering, contributing to the evidence base that underpins clinical practice and public health initiatives. Each of these graduate pathways offers a unique way to contribute to the fight against cardiovascular disease.
PhD/Research Focuses: Molecular Cardiology, Epidemiology
For those drawn to the investigative aspects of cardiovascular disease, pursuing a Ph.D. or engaging in dedicated research offers an opportunity to contribute to the cutting edge of knowledge. Within biomedical research, several specialized focuses are particularly relevant to CVD. Molecular Cardiology is a field that delves into the genetic, molecular, and cellular mechanisms underlying heart function and disease. Researchers in this area might investigate how specific genes contribute to congenital heart defects, explore the signaling pathways involved in cardiac hypertrophy (heart enlargement), or develop gene therapies for inherited cardiomyopathies.
Another critical research focus is Epidemiology, specifically cardiovascular epidemiology. Epidemiologists study the distribution, patterns, and determinants of health and disease conditions in defined populations. In the context of CVD, this involves identifying risk factors (like diet, exercise, smoking, and environmental exposures), tracking the incidence and prevalence of different heart conditions, evaluating the effectiveness of preventive interventions, and understanding health disparities across different demographic groups. Their findings are essential for informing public health policies and clinical guidelines. You can explore more about this field through Health & Medicine courses.
Other research areas include, but are not limited to, cardiovascular pharmacology (developing and testing new drugs), bioengineering (designing medical devices like artificial heart valves or stents), and imaging sciences (advancing diagnostic techniques). These research focuses are often interdisciplinary, requiring collaboration across various scientific fields to tackle the complex challenges posed by cardiovascular disease. A strong grounding in research methodology, statistical analysis, and scientific communication is paramount for success in these demanding yet highly impactful areas.
Clinical Training Requirements (e.g., Medical School, Residencies)
The path to becoming a clinical practitioner in cardiovascular health, such as a cardiologist, is lengthy and rigorous, demanding extensive education and hands-on training. The journey typically begins with completing a bachelor's degree with specific prerequisite courses, primarily in biology and chemistry. Following this, aspiring physicians must gain admission to medical school, which is a four-year program. Medical school curricula cover a broad range of medical sciences, including anatomy, physiology, pharmacology, pathology, and an introduction to clinical medicine.
After graduating from medical school with an M.D. (Doctor of Medicine) or D.O. (Doctor of Osteopathic Medicine) degree, the next step is a residency program. For those aiming for cardiology, this usually involves a three-year residency in internal medicine. During residency, physicians receive supervised training in various hospital and clinic settings, gaining experience in diagnosing and managing a wide array of adult medical conditions. This period is crucial for developing core clinical competencies.
Upon successful completion of an internal medicine residency, physicians who wish to specialize further in heart-related conditions must then undertake a cardiology fellowship. This is typically an additional three years of specialized training focused exclusively on cardiovascular diseases, including diagnostic techniques, treatment modalities, and patient management. Some cardiologists may pursue even further sub-specialization through additional fellowship training in areas like interventional cardiology, electrophysiology, or heart failure. The entire process, from starting medical school to completing a cardiology fellowship, generally takes at least 10-14 years.
These books are foundational texts in the field of cardiology and cardiovascular medicine, offering comprehensive knowledge for students and practitioners.
Online Learning and Skill Development
In today's rapidly evolving educational landscape, online learning has emerged as a valuable tool for acquiring knowledge and developing skills in numerous fields, including aspects of cardiovascular health. Whether you are a self-directed learner, a professional seeking to pivot your career, or someone looking to supplement formal education, online courses and resources can offer flexible and accessible learning opportunities. This section explores how online platforms can be utilized for self-study in core topics, project-based learning, and integration with traditional educational pathways, while also acknowledging the limitations of non-accredited training for certain career goals.
For those embarking on a learning journey in cardiovascular health, especially if you're new to the field or considering a career change, the prospect can seem daunting. Remember that every expert started somewhere, and online resources can provide a supportive and structured way to begin. Take advantage of the flexibility to learn at your own pace and build a solid foundation. OpenCourser allows learners to easily browse through thousands of courses in Health & Medicine, save interesting options to a list, compare syllabi, and read summarized reviews to find the perfect online course.
Core Topics for Self-Study (e.g., ECG Interpretation, Lipid Metabolism)
Online platforms offer a wealth of resources for self-study in foundational topics relevant to cardiovascular health. For individuals interested in understanding the heart's electrical activity, courses on ECG (Electrocardiogram) interpretation are widely available. These courses can teach learners how to read and understand ECG tracings, identify normal rhythms, and recognize patterns indicative of various cardiac conditions such as arrhythmias, myocardial ischemia, and electrolyte imbalances. While online learning cannot replace hands-on clinical experience, it can provide a strong theoretical understanding and familiarity with common ECG findings.
Another crucial area amenable to online self-study is lipid metabolism. Understanding how the body processes fats and cholesterol is fundamental to comprehending conditions like atherosclerosis and hyperlipidemia. Online courses can cover the biochemistry of lipids, the different types of lipoproteins (e.g., LDL, HDL), their roles in health and disease, and the mechanisms by which lipid-lowering medications work. This knowledge is vital for anyone involved in preventive cardiology, nutrition, or cardiovascular research.
Other core topics that can be effectively explored through online learning include basic cardiovascular anatomy and physiology, the pharmacology of common cardiovascular drugs, principles of hemodynamics, and an introduction to cardiovascular risk factors and prevention strategies. Many platforms provide interactive modules, video lectures, and self-assessment quizzes to enhance the learning experience. These resources can be particularly beneficial for students preparing for more advanced studies, healthcare professionals seeking to refresh their knowledge, or individuals with a keen interest in understanding cardiovascular health.
The following courses can help build a foundation in understanding broad public health strategies related to chronic diseases, including those impacting cardiovascular health.
Project-Based Learning: Case Study Analyses, Virtual Labs
Project-based learning offers a dynamic and engaging way to apply theoretical knowledge gained from online courses to more practical scenarios in the context of cardiovascular disease. Many online platforms and educational programs are incorporating projects like case study analyses. These exercises present learners with detailed patient scenarios, including medical history, symptoms, diagnostic test results, and treatment plans related to various cardiovascular conditions. Students are then tasked with analyzing the information, formulating potential diagnoses, considering treatment options, and discussing management strategies. This approach helps develop critical thinking, problem-solving, and decision-making skills in a simulated clinical context.
The advent of virtual labs and simulations provides another avenue for experiential learning online. While not a substitute for physical lab work in all disciplines, virtual labs can offer interactive experiences in areas like physiology or pharmacology. For example, learners might be able to simulate the effects of different drugs on cardiac parameters, explore a 3D anatomical model of the heart, or practice interpreting simulated diagnostic outputs like echocardiograms or angiograms. These tools can make complex concepts more tangible and accessible, particularly for visual and kinesthetic learners.
Furthermore, some online courses may encourage or require learners to undertake small research projects, literature reviews, or public health campaign designs related to cardiovascular disease prevention or awareness. Such projects allow students to delve deeper into specific areas of interest, develop research and communication skills, and contribute, even in a small way, to the broader understanding or dissemination of knowledge about CVD. Engaging in these types of projects can significantly enhance the learning experience and provide a more comprehensive understanding of the multifaceted nature of cardiovascular health.
Integration with Formal Education Pathways
Online learning can serve as a powerful supplement to formal education pathways in cardiovascular health, offering flexibility and access to a wide range of specialized topics. University students pursuing degrees in biology, pre-medicine, nursing, or allied health sciences can use online courses to deepen their understanding of specific cardiovascular concepts that may only be touched upon in their core curriculum. For instance, a student finding traditional lectures on cardiac physiology challenging might benefit from an engaging online course with interactive animations and detailed explanations.
For those already in medical school or postgraduate training programs, online resources can be invaluable for board exam preparation, learning about the latest research advancements, or exploring subspecialties within cardiology. Many professional organizations and academic institutions offer online modules, webinars, and virtual conferences that provide continuing medical education (CME) credits and keep practitioners abreast of new guidelines and treatment modalities. This continuous learning is essential in a rapidly evolving field like cardiovascular medicine.
Moreover, online courses can bridge gaps in knowledge for individuals transitioning between different roles or disciplines within the broader healthcare sector. A nurse wanting to specialize in cardiac care, or a researcher from a different biological science aiming to focus on cardiovascular studies, can use targeted online learning to acquire specific foundational knowledge before or during their formal transition. OpenCourser's Learner's Guide offers valuable articles on how to effectively structure self-learning and integrate online courses with existing educational pursuits, helping learners make the most of these resources.
These courses offer insights into lifestyle factors and therapeutic approaches relevant to cardiovascular health, which can complement formal medical or health sciences education.
Limitations of Non-Accredited Training
While online learning offers numerous benefits, it's crucial to understand the limitations, particularly of non-accredited training, when considering careers that require formal licensure or certification, such as becoming a physician, nurse, or certified technologist. Non-accredited courses, while potentially rich in information and excellent for foundational knowledge or personal development, typically do not fulfill the stringent educational requirements set by licensing bodies and professional credentialing organizations. For roles that involve direct patient care and clinical decision-making, accredited degree programs and supervised clinical experience are indispensable.
One of the primary limitations is the lack of formal validation of skills and knowledge. Accredited programs undergo rigorous review processes to ensure they meet specific educational standards, including curriculum content, faculty qualifications, and student assessment methods. This accreditation provides an assurance of quality and prepares graduates to meet professional practice standards. Non-accredited training often lacks this external validation, making it difficult for employers or licensing boards to gauge the learner's competency reliably, especially for complex clinical skills like performing diagnostic procedures or prescribing treatments.
Furthermore, hands-on clinical experience under the supervision of qualified professionals is a cornerstone of training for most healthcare roles related to cardiovascular disease. This practical component, which is integral to accredited programs, cannot be fully replicated by online courses alone, especially those without a structured, in-person clinical practicum. Therefore, while online learning is a valuable tool for supplementing education, refreshing knowledge, or exploring areas of interest, individuals aiming for licensed clinical professions must pursue formal, accredited educational pathways. It's essential to research the specific educational and credentialing requirements for your desired career path in cardiovascular health to make informed decisions about your learning journey.
Career Progression in Cardiovascular Fields
The field of cardiovascular health offers a diverse range of career paths with opportunities for growth and specialization. Whether starting in an entry-level position or aiming for leadership roles, understanding the potential for progression is key for career planning. This section will explore typical career trajectories, from initial roles to mid-career advancements and leadership opportunities, as well as emerging niches within this dynamic sector. For those embarking on this journey, particularly early-career professionals, remember that continuous learning and adaptability are vital. The landscape of cardiovascular medicine is always evolving, and embracing new knowledge and skills will be crucial for long-term success and fulfillment.
Entry-Level Roles: Clinical Assistants, Research Technicians
For individuals beginning their careers in cardiovascular health, several entry-level roles provide valuable experience and a foundation for future advancement. Clinical Assistants, often working in cardiology clinics or hospital departments, support physicians and nurses with patient care. Their responsibilities might include taking patient histories, measuring vital signs, preparing patients for examinations or procedures, performing basic diagnostic tests like EKGs, and managing patient records. These roles offer direct patient interaction and exposure to the clinical environment, which can be an excellent stepping stone for those considering further education in nursing, medicine, or as a physician assistant.
Research Technicians play a crucial role in academic institutions, pharmaceutical companies, or research organizations conducting studies related to cardiovascular disease. They typically work under the supervision of principal investigators (scientists or physicians) and assist with laboratory experiments, data collection and analysis, maintaining lab equipment, and ensuring compliance with research protocols. This path is well-suited for individuals with a strong background in biology or chemistry who are interested in the scientific discovery process. Experience as a research technician can be valuable for those planning to pursue graduate studies (M.S. or Ph.D.) in biomedical sciences or for entry into medical school with a research focus.
Other entry-level positions might include phlebotomists specializing in cardiac patients, medical scribes in cardiology practices, or patient service representatives in cardiovascular units. These roles, while varied, all contribute to the broader ecosystem of cardiovascular care and research, providing essential skills and insights into the field. Many cardiovascular technologists also begin in entry-level positions, performing diagnostic tests like echocardiograms or stress tests after completing an associate's degree or certificate program.
Mid-Career Paths: Specialized Clinicians, Lab Directors
As professionals in the cardiovascular field gain experience and often further education or certifications, a variety of mid-career paths open up, offering greater responsibility and specialization. Specialized Clinicians emerge after years of dedicated training and practice. For example, cardiologists may sub-specialize in areas like interventional cardiology (performing procedures like angioplasty and stenting), electrophysiology (diagnosing and treating heart rhythm disorders), advanced heart failure and transplant cardiology, or non-invasive cardiology (focusing on imaging techniques). Similarly, experienced nurses can become Clinical Nurse Specialists or Nurse Practitioners specializing in cardiac care, managing complex patient cases and often leading nursing teams.
In the research and diagnostic realm, individuals may advance to roles such as Lab Directors or managers. A Lab Director in a cardiac catheterization lab, echocardiography lab, or a cardiovascular research laboratory oversees the daily operations, ensures quality control and compliance with regulations, manages staff, and may also be involved in budget planning and implementing new technologies or protocols. This requires not only technical expertise but also strong leadership, organizational, and communication skills.
Other mid-career opportunities include roles in pharmaceutical or medical device companies as medical science liaisons, clinical trial managers, or product specialists. Experienced cardiovascular technologists might become lead technologists or supervisors in their departments. Public health professionals could lead specific cardiovascular disease prevention programs at local, state, or national levels. These mid-career roles often involve a blend of advanced technical skills, leadership, and a deeper focus within a particular niche of cardiovascular health.
Leadership Opportunities: Hospital Administration, Policy Advocacy
With significant experience and often advanced degrees or specialized training, professionals in the cardiovascular field can ascend to influential leadership positions. Within healthcare institutions, opportunities in Hospital Administration are common. Individuals with a clinical background in cardiology, cardiovascular surgery, or nursing, perhaps combined with a Master's in Health Administration (MHA) or Business Administration (MBA), might become directors of cardiovascular service lines, chief medical officers, or even hospital CEOs. These roles involve strategic planning, financial management, quality improvement initiatives, and leading large teams of healthcare professionals to ensure the delivery of high-quality cardiovascular care.
Beyond the hospital walls, leadership roles in Policy Advocacy offer a chance to shape the broader landscape of cardiovascular health. Experienced clinicians, researchers, or public health experts may work for government agencies (like the Centers for Disease Control and Prevention or the National Institutes of Health), non-profit organizations (such as the American Heart Association), or professional societies. In these capacities, they might influence health policy by developing clinical guidelines, advocating for legislation that supports cardiovascular health (e.g., tobacco control, healthy food initiatives), and allocating resources for research and prevention programs. Their expertise is crucial in translating scientific evidence into actionable public health strategies.
Other leadership opportunities include becoming a principal investigator leading a major research program, a dean or department chair in an academic institution, or an executive in a pharmaceutical or medical device company. These positions require a strong vision, exceptional leadership skills, and a deep understanding of the complexities of the cardiovascular field. They offer the potential to make a broad and lasting impact on preventing and treating cardiovascular disease at a systemic level.
Emerging Niches: Digital Health, Preventive Cardiology
The field of cardiovascular medicine is continuously evolving, with technological advancements and new research insights giving rise to exciting emerging niches. Digital Health is one such rapidly expanding area. This encompasses the use of technologies like wearable devices, mobile health apps, artificial intelligence (AI), and telehealth to monitor, diagnose, and manage cardiovascular conditions. Professionals in this niche might develop AI algorithms to analyze cardiac images or predict heart attack risk, design mobile apps to help patients manage their blood pressure or adhere to medication, or implement telehealth programs for remote cardiac rehabilitation. This area requires a blend of clinical knowledge and technological expertise.
Preventive Cardiology is gaining increasing prominence as the focus shifts from solely treating established disease to proactively mitigating risk factors and preventing CVD from developing in the first place. While prevention has always been a part of cardiology, dedicated preventive cardiology programs and specialists are becoming more common. These professionals focus on comprehensive risk assessment, lifestyle counseling (diet, exercise, smoking cessation), management of risk factors like hypertension and hyperlipidemia in at-risk populations, and utilizing advanced screening tools to identify early signs of disease. This niche appeals to those passionate about public health and long-term patient well-being.
Other emerging areas include cardio-oncology (managing cardiovascular complications in cancer patients), inherited cardiac conditions (focusing on genetic heart diseases), and advances in regenerative medicine and gene therapy for heart repair. These specialized fields often require additional training and offer opportunities to work at the forefront of medical innovation. As our understanding of cardiovascular disease deepens and technology continues to advance, these and other niches will likely continue to grow, offering diverse and impactful career paths for future generations of cardiovascular health professionals. Exploring Technology courses can provide foundational knowledge for those interested in the digital health aspect.
Innovations and Trends in Cardiovascular Disease Management
The landscape of cardiovascular disease management is dynamic, characterized by continuous innovation and evolving trends. Advances in technology, a deeper understanding of disease mechanisms, and a growing emphasis on personalized and preventive medicine are shaping the future of cardiac care. This section will highlight some of the key innovations and trends, including the role of artificial intelligence in diagnostics, breakthroughs in gene therapy and regenerative medicine, the impact of wearable technology, and the influence of broader environmental factors like climate change on CVD epidemiology.
AI in Diagnostics (e.g., Imaging Analysis)
Artificial intelligence (AI) is rapidly transforming cardiovascular diagnostics, particularly in the realm of imaging analysis. AI algorithms, especially those based on machine learning and deep learning, are demonstrating remarkable capabilities in interpreting complex medical images such as echocardiograms, cardiac MRIs, CT scans, and angiograms. These algorithms can be trained on vast datasets to identify subtle patterns and anomalies that might be missed by the human eye, potentially leading to earlier and more accurate diagnoses.
For example, AI can assist in quantifying cardiac function, such as measuring ejection fraction from an echocardiogram, with greater speed and consistency than manual methods. It can also help in detecting early signs of coronary artery disease by analyzing CT angiograms for plaque buildup or identifying structural abnormalities in cardiac MRI. Beyond image interpretation, AI is also being explored for risk stratification, predicting which patients are at higher risk of developing specific cardiovascular conditions or experiencing adverse events based on a combination of imaging data, electronic health records, and genetic information.
The integration of AI into diagnostic workflows holds the promise of improving efficiency, reducing inter-observer variability, and ultimately enhancing patient outcomes. However, the development and implementation of AI in cardiovascular diagnostics also come with challenges, including the need for large, diverse, and well-curated datasets for training, ensuring algorithmic fairness and transparency, and addressing regulatory and ethical considerations. As AI technology continues to mature, it is poised to become an indispensable tool for clinicians in the fight against cardiovascular disease. Professionals interested in this intersection can benefit from exploring Artificial Intelligence courses.
This course offers insights into advanced cardiac imaging techniques, a field increasingly impacted by AI.
Gene Therapy and Regenerative Medicine Advances
The fields of gene therapy and regenerative medicine hold immense promise for revolutionizing the treatment of cardiovascular diseases, particularly those with a strong genetic basis or involving significant tissue damage. Gene therapy aims to treat or cure diseases by modifying a person's genes. In the context of CVD, researchers are exploring gene therapies for inherited cardiomyopathies (diseases of the heart muscle), familial hypercholesterolemia (a genetic condition causing very high cholesterol), and even to promote the growth of new blood vessels (angiogenesis) in ischemic heart tissue.
Approaches in gene therapy can involve replacing a mutated gene that causes disease with a healthy copy, inactivating or "knocking out" a mutated gene that is functioning improperly, or introducing a new gene into the body to help fight a disease. While still largely in experimental stages for many cardiovascular applications, significant progress is being made, with some therapies advancing to clinical trials. The development of safer and more efficient gene delivery vectors (often modified viruses) is a key area of ongoing research.
Regenerative medicine focuses on repairing or replacing damaged tissues and organs. For cardiovascular disease, this often involves strategies to regenerate heart muscle lost after a heart attack. Approaches include using stem cells (undifferentiated cells with the potential to develop into various cell types) to repopulate damaged areas of the heart, stimulating the heart's own (limited) regenerative capacity, or tissue engineering to create cardiac patches or even whole heart structures. While challenges remain in terms of cell survival, integration, and function, the potential to restore heart function through regenerative approaches offers hope for patients with severe heart failure and other debilitating conditions.
Wearable Technology for Patient Monitoring
Wearable technology has emerged as a significant trend in cardiovascular disease management, empowering both patients and clinicians with continuous physiological data. Devices like smartwatches, fitness trackers, and specialized medical-grade wearables can monitor a variety of cardiovascular parameters, including heart rate, heart rhythm (via ECG capabilities), blood oxygen saturation, physical activity levels, and even blood pressure in some newer models.
This continuous stream of data offers several benefits. For patients, it can increase awareness of their own health status, motivate lifestyle changes, and facilitate early detection of potential issues. For instance, many smartwatches can now detect irregular heart rhythms suggestive of atrial fibrillation, prompting users to seek medical attention. For clinicians, wearable data can provide a more comprehensive picture of a patient's cardiovascular health outside of traditional clinic visits, aiding in diagnosis, treatment titration, and long-term management of chronic conditions like hypertension or heart failure.
However, the integration of wearable technology into clinical practice also presents challenges. These include ensuring data accuracy and reliability, managing the large volume of data generated, addressing data privacy and security concerns, and ensuring equitable access to these technologies. Clinical validation and clear guidelines for interpreting and acting upon wearable data are crucial. Despite these hurdles, wearable technology is poised to play an increasingly important role in proactive and personalized cardiovascular care, shifting the paradigm towards more continuous and patient-centered monitoring.
These books delve into various aspects of heart disease, including diagnostic and treatment modalities that are increasingly being supplemented by wearable monitoring technologies.
Impact of Climate Change on CVD Epidemiology
A growing body of evidence indicates that climate change is having, and will continue to have, a significant impact on the epidemiology of cardiovascular disease. Extreme weather events, rising temperatures, and air pollution, all exacerbated by climate change, can directly and indirectly affect cardiovascular health. For example, heatwaves can put a strain on the cardiovascular system, increasing the risk of heart attacks, strokes, and exacerbation of heart failure, particularly in vulnerable populations such as the elderly and those with pre-existing heart conditions.
Air pollution, which is often worsened by climate change-related factors like wildfires and stagnant air masses, is a well-established risk factor for CVD. Fine particulate matter (PM2.5) and other pollutants can trigger inflammation, oxidative stress, and endothelial dysfunction, contributing to atherosclerosis, hypertension, and arrhythmias. Changes in temperature and precipitation patterns can also affect the distribution of vector-borne diseases, some of which can have cardiac complications. Furthermore, climate change can impact food security and nutrition, potentially leading to dietary shifts that increase CVD risk.
Understanding these linkages is crucial for public health planning and developing adaptation strategies to protect cardiovascular health in a changing climate. This includes strengthening early warning systems for extreme weather, implementing policies to reduce air pollution, promoting climate-resilient health systems, and raising awareness among healthcare professionals and the public about the cardiovascular risks associated with climate change. The intersection of climate change and health is an emerging area of research and policy, highlighting the interconnectedness of environmental and human well-being. Further exploration can be done through Environmental Sciences courses.
Ethical Challenges in Cardiovascular Care
The practice of cardiovascular medicine, while offering immense benefits, is not without its ethical complexities. Advances in technology, resource limitations, and the profound impact of cardiovascular disease on individuals and families give rise to a range of challenging ethical dilemmas. This section is intended for a broad audience, including researchers, policymakers, students of ethics, and practitioners, to foster an understanding of these moral considerations. We will explore issues such as resource allocation, genetic testing controversies, end-of-life care decisions, and equity in clinical trials.
Resource Allocation in Low-Income Regions
One of the most pressing ethical challenges in global cardiovascular care is the equitable allocation of limited healthcare resources, particularly in low-income regions. Cardiovascular diseases impose a heavy burden on these regions, yet access to essential diagnostic tools, medications, advanced procedures, and trained personnel is often severely restricted due to financial constraints and underdeveloped health infrastructure. This disparity raises fundamental questions about justice and the right to health.
Decisions regarding resource allocation often involve difficult choices. For example, should limited funds be prioritized for primary prevention strategies that benefit a larger population in the long term, or for expensive, life-saving interventions for a smaller number of individuals with acute conditions? How can access to essential cardiovascular medicines, such as those for hypertension or heart failure, be ensured when they may be unaffordable for many patients or healthcare systems? The development and implementation of cost-effective interventions are critical, but even then, scarcity may necessitate rationing of care, leading to ethical dilemmas about who receives treatment when not everyone can.
Addressing these challenges requires a multi-pronged approach. This includes advocating for increased investment in health systems in low-income countries, promoting the development and adoption of affordable and appropriate technologies, fostering international collaborations and partnerships, and ensuring that resource allocation decisions are made transparently and ethically, with input from local communities and healthcare providers. The World Health Organization (WHO) and other international bodies play a role in supporting governments to tackle these issues.
Genetic Testing Controversies
The increasing availability and decreasing cost of genetic testing have brought both promise and ethical controversies to the field of cardiovascular medicine. Genetic testing can identify individuals at increased risk for certain inherited cardiovascular conditions, such as hypertrophic cardiomyopathy, long QT syndrome, or familial hypercholesterolemia. This information can potentially guide preventive strategies, inform treatment decisions, and allow for cascade screening of family members who may also be at risk.
However, the use of genetic testing in CVD also raises several ethical concerns. One major issue is the potential for genetic discrimination, where individuals with identified genetic predispositions might face discrimination from employers or insurance companies. While laws exist in some countries to protect against this, concerns persist. Another challenge is the interpretation of genetic test results, especially for variants of uncertain significance (VUS), where it's unclear whether a specific genetic change is truly disease-causing. This can lead to anxiety and uncertainty for patients and their families, and potentially to unnecessary medical interventions.
Furthermore, questions arise about informed consent, genetic counseling, privacy, and data security. Patients need to fully understand the implications of genetic testing, including the potential psychological and social consequences, before undergoing testing. Access to genetic counseling is crucial to help individuals interpret complex results and make informed decisions. Ensuring the confidentiality of sensitive genetic information and preventing its misuse are also paramount. As genetic technologies continue to advance, ongoing ethical debate and robust regulatory frameworks are needed to navigate these complex issues responsibly.
End-of-Life Care Decisions
Cardiovascular disease is a leading cause of mortality, and as such, end-of-life care decisions are a frequent and often ethically challenging aspect of cardiovascular medicine. For patients with advanced, life-limiting heart conditions, such as end-stage heart failure or severe, untreatable coronary artery disease, discussions about prognosis, goals of care, and preferences for end-of-life interventions become critically important.
Ethical dilemmas can arise concerning the use of life-sustaining treatments, such as mechanical ventilation, implantable cardioverter-defibrillators (ICDs), or ventricular assist devices (VADs). While these technologies can prolong life, they may not always improve quality of life and can sometimes lead to prolonged suffering. Decisions about initiating, withholding, or withdrawing such treatments require careful consideration of the patient's values, preferences, and understanding of their condition, as well as the medical realities. Advance care planning, including the completion of advance directives and the appointment of a healthcare proxy, can help ensure that a patient's wishes are respected if they lose the capacity to make decisions for themselves.
Communication between healthcare providers, patients, and families is paramount in navigating these sensitive situations. Honest and compassionate discussions about prognosis, the potential benefits and burdens of different treatment options, and palliative care services are essential. Palliative care, which focuses on relieving symptoms and improving quality of life for patients with serious illnesses, should be integrated early in the course of advanced heart disease, not just in the final days or weeks of life. Ensuring patient autonomy, promoting shared decision-making, and providing comprehensive psychosocial and spiritual support are key ethical considerations in providing high-quality end-of-life care for individuals with cardiovascular disease.
Clinical Trial Equity Issues
Clinical trials are the cornerstone of evidence-based medicine, providing the data needed to determine the safety and efficacy of new cardiovascular drugs, devices, and interventions. However, ethical issues related to equity in clinical trials are a significant concern. Historically, many cardiovascular clinical trials have underrepresented certain populations, including women, older adults, and individuals from racial and ethnic minority groups. This lack of diversity can limit the generalizability of trial results and may lead to treatments that are less effective or have different side effect profiles in these underrepresented groups.
Ensuring equitable access to participation in clinical trials is another ethical imperative. Barriers to participation can include restrictive eligibility criteria, lack of awareness about trial opportunities, geographic limitations, financial constraints (e.g., travel costs, time off work), and mistrust of the medical research system, particularly among historically marginalized communities. Efforts are needed to design more inclusive trials, actively recruit diverse participants, and address these barriers to ensure that the benefits of research are shared more broadly.
Furthermore, ethical considerations extend to the conduct of clinical trials in low- and middle-income countries (LMICs). While conducting research in these settings can be important for addressing global health needs, it is crucial to ensure that trials are ethically sound, that participants are protected from exploitation, and that the research is relevant to the health needs of the local population. This includes ensuring appropriate informed consent processes, providing access to proven effective treatments for control groups, and making plans for post-trial access to beneficial interventions. Striving for greater equity in all aspects of cardiovascular clinical trials is essential for advancing science and improving health outcomes for all populations.
Global Perspectives on Cardiovascular Disease
Cardiovascular disease is not confined by borders; it is a truly global challenge that affects populations in diverse ways across the world. Understanding these global perspectives is crucial for anyone involved in international health, public health policy, or research with a worldwide scope. This section will explore regional prevalence patterns, the influence of culture on prevention strategies, the importance of cross-border research collaborations, and the role of major international initiatives in combating CVD.
Regional Prevalence Patterns (e.g., LMIC vs. High-Income Countries)
The prevalence and impact of cardiovascular disease vary significantly across different regions of the world, with notable distinctions between low- and middle-income countries (LMICs) and high-income countries (HICs). While CVD was once considered primarily a disease of affluence, it is now the leading cause of death globally, with over three-quarters of CVD deaths occurring in LMICs. This shift reflects complex changes in lifestyle, diet, urbanization, and population aging in these regions.
In many HICs, while CVD remains a major health issue, mortality rates from conditions like coronary heart disease and stroke have seen declines in recent decades. This is often attributed to better public health interventions (e.g., tobacco control, promotion of healthy diets), advancements in medical treatments (e.g., statins, reperfusion therapies for heart attacks), and improved healthcare access. However, risk factors like obesity and diabetes are on the rise in some HICs, posing ongoing challenges.
In contrast, many LMICs face a "double burden" of disease, grappling with both infectious diseases and a rapidly increasing prevalence of non-communicable diseases (NCDs) like CVD. Risk factors such as tobacco use, unhealthy diets (often characterized by increased consumption of processed foods high in salt, sugar, and unhealthy fats), and physical inactivity are becoming more common. Furthermore, healthcare systems in LMICs are often less equipped to manage chronic conditions like CVD, with limited access to diagnostic tools, essential medicines, and specialized care. Rheumatic heart disease, a consequence of untreated streptococcal infections, also remains a significant problem primarily in LMICs.
These courses provide insight into global health challenges and strategies, including those related to non-communicable diseases like CVD.
Cultural Influences on Prevention Strategies
Cultural factors play a significant role in shaping behaviors, beliefs, and practices related to health, and therefore have a profound influence on the effectiveness of cardiovascular disease prevention strategies. What constitutes a "healthy diet," acceptable levels of physical activity, attitudes towards smoking and alcohol consumption, and health-seeking behaviors can vary widely across different cultures. Therefore, one-size-fits-all prevention programs are often less effective than those tailored to specific cultural contexts.
For example, dietary recommendations must consider traditional foods, cooking methods, and meal patterns. Promoting a Mediterranean-style diet might be well-received in some cultures but less applicable in others where staple foods and culinary traditions differ. Similarly, messages about physical activity need to be culturally sensitive, considering gender norms, available infrastructure, and preferred types of activities. In some cultures, community-based group activities might be more successful than individual exercise regimens.
Beliefs about the causes of illness and the role of traditional or alternative medicine can also influence adherence to preventive measures and engagement with Western medical systems. Effective prevention strategies often involve working closely with community leaders, cultural influencers, and local health workers to develop messages and interventions that resonate with the target population. Understanding and respecting cultural nuances is essential for building trust and fostering sustainable behavior change to reduce the burden of cardiovascular disease globally. Health education is a related field that often considers these cultural factors.
This course on the New Nordic Diet touches upon how dietary concepts are linked to cultural and health aspects.
Cross-Border Research Collaborations
Addressing the global challenge of cardiovascular disease necessitates robust cross-border research collaborations. These partnerships bring together diverse expertise, resources, and perspectives, fostering innovation and accelerating the translation of research findings into practice. International collaborations are particularly vital for studying diseases that have varying prevalence or unique risk factor profiles in different populations, allowing for comparative analyses and a deeper understanding of the interplay between genetics, environment, and lifestyle.
Collaborative research can take many forms, including multi-center clinical trials, epidemiological studies involving diverse cohorts, joint laboratory research projects, and shared data platforms. Such initiatives can lead to the development of more globally relevant diagnostic tools, treatments, and prevention strategies. For instance, international efforts to identify genetic markers for CVD across different ethnic groups can enhance our understanding of disease susceptibility and inform personalized medicine approaches worldwide.
Funding agencies, academic institutions, and non-governmental organizations play a crucial role in facilitating and supporting these cross-border collaborations. However, such partnerships also come with challenges, including navigating different regulatory environments, addressing ethical considerations related to data sharing and intellectual property, and overcoming logistical and communication barriers. Despite these hurdles, the benefits of pooling global talent and resources to tackle a common enemy like cardiovascular disease are immense, leading to more impactful research and ultimately better health outcomes for people around the world.
WHO Initiatives and Sustainable Development Goals
The World Health Organization (WHO) plays a central leadership role in global efforts to combat cardiovascular disease. Recognizing CVD as a major public health crisis, the WHO develops global strategies, provides technical support to countries, and monitors trends to inform action. A key component of their work is the Global Hearts Initiative, launched in collaboration with the U.S. Centers for Disease Control and Prevention (CDC) and other partners. This initiative provides a set of evidence-based technical packages to help governments strengthen CVD prevention and control, focusing on areas like tobacco control (MPOWER), salt reduction (SHAKE), management of CVD in primary healthcare (HEARTS), and eliminating trans fats (REPLACE).
The fight against cardiovascular disease is also intrinsically linked to the broader United Nations' Sustainable Development Goals (SDGs), particularly SDG 3, which aims to "ensure healthy lives and promote well-being for all at all ages." Target 3.4 of the SDGs specifically calls for a one-third reduction in premature mortality from non-communicable diseases (NCDs), including CVD, by 2030, through prevention and treatment. Achieving this target requires comprehensive action across multiple sectors, addressing not only the direct risk factors for CVD but also the social, economic, and environmental determinants of health.
WHO initiatives and the SDG framework emphasize the importance of universal health coverage to ensure that everyone has access to quality essential healthcare services, including those for CVD prevention and management, without facing financial hardship. They also highlight the need for multi-sectoral collaboration, involving governments, civil society, the private sector, and international organizations, to create environments that promote heart health. These global frameworks provide a roadmap and a platform for coordinated action to reduce the devastating global burden of cardiovascular disease.
Diagnostic Tools and Treatment Modalities
The diagnosis and treatment of cardiovascular disease rely on a sophisticated array of tools and therapeutic approaches. From advanced imaging techniques that allow clinicians to visualize the heart and blood vessels in remarkable detail, to life-saving invasive procedures and a wide range of pharmacological interventions, the options for managing CVD are continually expanding. This section, aimed at practitioners, trainees, and researchers, will explore key diagnostic modalities and treatment strategies, including imaging, invasive procedures, drug therapies, and the critical role of lifestyle modification frameworks.
Imaging Techniques: Echocardiography, Cardiac MRI
Cardiac imaging plays a pivotal role in the diagnosis, assessment, and management of a wide spectrum of cardiovascular diseases. Among the most commonly used non-invasive techniques are echocardiography and cardiac magnetic resonance imaging (CMR). Echocardiography utilizes ultrasound waves to create real-time images of the heart. It can assess the heart's chambers, valves, walls, and the pumping action of the heart muscle. Doppler echocardiography can also measure the speed and direction of blood flow within the heart. Transthoracic echocardiography (TTE), where the ultrasound probe is placed on the chest, is the standard approach, while transesophageal echocardiography (TEE), involving a probe passed into the esophagus, provides clearer images of certain heart structures.
Cardiac Magnetic Resonance (CMR) imaging uses powerful magnets, radio waves, and a computer to produce detailed still and moving images of the heart and blood vessels. CMR is excellent for assessing heart structure and function, evaluating blood flow, detecting scar tissue (e.g., after a heart attack), and diagnosing a variety of conditions including cardiomyopathies, congenital heart disease, and pericardial diseases. It offers superior soft tissue contrast compared to other imaging modalities and does not use ionizing radiation. Other important imaging techniques include cardiac computed tomography (CT), particularly CT coronary angiography (CTCA) for visualizing coronary arteries, and nuclear cardiology techniques like SPECT and PET scans, which assess blood flow and metabolic activity of the heart muscle.
These diverse imaging tools provide complementary information, and the choice of technique depends on the specific clinical question being addressed. Advances in imaging technology, including 3D imaging and AI-assisted analysis, continue to enhance their diagnostic capabilities.
This course offers an in-depth look at Cardiac Magnetic Resonance (CMR), a key imaging modality.
This book provides a detailed guide to an invasive imaging and therapeutic technique.
Invasive Procedures: Angioplasty, Bypass Surgery
For certain cardiovascular conditions, particularly those involving significant blockages in the coronary arteries, invasive procedures are often necessary to restore blood flow and improve outcomes. Two cornerstone interventions are angioplasty (often with stenting) and coronary artery bypass graft (CABG) surgery. Angioplasty, also known as percutaneous coronary intervention (PCI), is a minimally invasive procedure used to open narrowed or blocked coronary arteries. During angioplasty, a thin tube (catheter) with a balloon at its tip is guided to the site of the blockage. The balloon is then inflated, compressing the plaque against the artery wall and widening the vessel. In most cases, a small, expandable mesh tube called a stent is then deployed at the site to help keep the artery open.
Coronary Artery Bypass Graft (CABG) surgery is a more invasive open-heart procedure typically recommended for patients with multiple severe blockages or when angioplasty is not suitable. In CABG, surgeons use a healthy blood vessel (graft) taken from another part of the patient's body (e.g., leg, chest, or arm) to create a new path for blood to flow around the blocked portion of the coronary artery. This effectively "bypasses" the blockage, restoring adequate blood supply to the heart muscle. The choice between angioplasty and CABG depends on various factors, including the number and location of blockages, the patient's overall health, and other coexisting medical conditions.
Other invasive procedures in cardiology include cardiac catheterization for diagnostic purposes (e.g., coronary angiography to visualize blockages), electrophysiology studies to diagnose and treat arrhythmias (which may involve ablation to destroy abnormal heart tissue causing the rhythm disturbance), and surgical repair or replacement of diseased heart valves. While these procedures carry inherent risks, they can be life-saving and significantly improve quality of life for appropriately selected patients.
This comprehensive text covers adult cardiac surgery, including procedures like bypass surgery.
Pharmacological Interventions: Anticoagulants, Statins
Pharmacological interventions are a cornerstone of cardiovascular disease management, used for prevention, treatment of acute events, and long-term control of chronic conditions. A vast array of medications is available, targeting different aspects of CVD pathophysiology. Anticoagulants, often referred to as blood thinners, work by interfering with the blood clotting process. They are used to prevent or treat conditions involving harmful blood clots, such as deep vein thrombosis (DVT), pulmonary embolism (PE), atrial fibrillation (to prevent stroke), and in patients with mechanical heart valves. Examples include warfarin and newer direct oral anticoagulants (DOACs).
Statins are a class of drugs that lower cholesterol levels in the blood, primarily by reducing the liver's production of cholesterol. High levels of LDL ("bad") cholesterol are a major risk factor for atherosclerosis. Statins are widely prescribed for primary prevention (in individuals at high risk of developing CVD) and secondary prevention (in those who have already had a cardiovascular event like a heart attack or stroke) to slow the progression of atherosclerosis and reduce the risk of future events.
Many other classes of drugs are vital in cardiovascular care. These include antiplatelet agents (like aspirin) which prevent platelets from clumping together to form clots; beta-blockers which slow heart rate and lower blood pressure; ACE inhibitors and angiotensin II receptor blockers (ARBs) which also lower blood pressure and are beneficial in heart failure; diuretics which help remove excess fluid from the body, reducing workload on the heart; and antiarrhythmic drugs to control abnormal heart rhythms. The selection and management of these medications require careful consideration of the patient's specific condition, risk factors, potential side effects, and drug interactions. Pharmacists play a key role in managing these complex medication regimens.
Lifestyle Modification Frameworks
While medical and surgical interventions are crucial, lifestyle modification remains a fundamental and powerful component of preventing and managing cardiovascular disease. Health organizations worldwide emphasize the importance of adopting heart-healthy behaviors. Comprehensive lifestyle modification frameworks typically focus on several key areas: diet, physical activity, smoking cessation, weight management, and stress reduction.
A heart-healthy diet generally involves consuming plenty of fruits, vegetables, whole grains, lean proteins (like fish and poultry), and healthy fats (like those found in olive oil and nuts), while limiting saturated and trans fats, cholesterol, sodium, red and processed meats, and added sugars. Regular physical activity is also paramount; guidelines often recommend at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic exercise per week, along with muscle-strengthening activities.
Smoking cessation is one of the most impactful lifestyle changes for cardiovascular health, as smoking significantly damages blood vessels and increases the risk of numerous CVDs. Maintaining a healthy weight through a combination of diet and exercise helps reduce strain on the heart and manage risk factors like hypertension and diabetes. Finally, effective stress management techniques, such as mindfulness, yoga, or regular exercise, can also contribute to better cardiovascular health, as chronic stress can negatively impact blood pressure and other risk factors. Healthcare providers play a critical role in educating patients about these lifestyle changes and supporting them in adopting and maintaining healthy habits. You can explore topics related to healthy eating through Food Sciences or Health & Fitness courses.
The following course offers guidance on lifestyle interventions that support overall health, including cardiovascular well-being.
Frequently Asked Questions (Career Focus)
Embarking on or navigating a career in fields related to cardiovascular disease can bring up many questions. This section aims to address some common queries that career-oriented individuals, from students to seasoned professionals considering a pivot, might have. We'll touch upon certifications, fellowship competitiveness, career transitions, industry opportunities beyond traditional healthcare, the impact of automation, and the value of international experience.
What entry-level certifications are most valued?
For many entry-level technical roles in cardiovascular health, specific certifications are highly valued and often required by employers. For aspiring Cardiovascular Technologists or Technicians, credentials from organizations like Cardiovascular Credentialing International (CCI) or the American Registry for Diagnostic Medical Sonography (ARDMS) are key. For example, CCI offers certifications such as Certified Cardiographic Technician (CCT) for those performing EKGs and stress tests, and Registered Cardiac Sonographer (RCS) or Registered Vascular Specialist (RVS) for those specializing in ultrasound imaging of the heart or blood vessels, respectively. ARDMS offers the Registered Diagnostic Cardiac Sonographer (RDCS) credential.
For individuals working in invasive cardiology settings, such as cardiac catheterization labs, the Registered Cardiovascular Invasive Specialist (RCIS) certification from CCI is often sought. These certifications typically require completion of an accredited educational program and/or a certain amount of clinical experience, followed by passing a comprehensive examination. They demonstrate a standardized level of knowledge and competence in the specific area of cardiovascular technology.
Beyond specific technologist roles, other entry-level positions might value different types of certifications. For example, medical assistants working in cardiology practices might benefit from a Certified Medical Assistant (CMA) or Registered Medical Assistant (RMA) credential. Phlebotomy technicians might seek certification from organizations like the American Society for Clinical Pathology (ASCP). While not always mandatory for every entry-level job, relevant certifications can significantly enhance employability, demonstrate commitment to the field, and may lead to better job prospects and potentially higher salaries. It's always advisable to research the specific requirements and preferred qualifications for the types of roles and employers you are interested in.
How competitive are cardiology fellowships?
Cardiology fellowships are widely regarded as highly competitive. After completing a demanding three-year internal medicine residency, physicians vying for a spot in a cardiology fellowship program face a rigorous application and selection process. The number of available fellowship positions is limited compared to the pool of qualified applicants, making it a challenging field to enter.
Several factors contribute to this competitiveness. Strong academic performance throughout medical school and residency, including high scores on standardized exams like the USMLE, is crucial. Research experience, publications, and presentations at medical conferences can significantly strengthen an application, demonstrating a commitment to advancing the field. Excellent letters of recommendation from supervising physicians and mentors who can attest to the applicant's clinical skills, work ethic, and potential as a cardiologist are also vital.
Furthermore, demonstrating a genuine interest and passion for cardiology through elective rotations, involvement in cardiology-related activities or societies, and a well-crafted personal statement can help an applicant stand out. The reputation of the residency program from which an applicant graduates can also play a role. Subspecialties within cardiology, such as interventional cardiology or electrophysiology, can be even more competitive, often requiring additional years of fellowship training after the general cardiology fellowship. Aspiring cardiologists should focus on building a strong, well-rounded application throughout their medical training to maximize their chances of securing a fellowship position in this demanding yet rewarding specialty.
Can I transition from nursing to cardiovascular research?
Yes, transitioning from a clinical nursing role to cardiovascular research is a feasible and increasingly common career path. Nurses, particularly those with experience in cardiac care units, bring a wealth of practical clinical knowledge, patient interaction skills, and an understanding of healthcare systems that can be invaluable in a research setting. There are several avenues for nurses to become involved in cardiovascular research.
One common role is that of a Clinical Research Nurse or Study Coordinator. In this capacity, nurses are often responsible for patient recruitment and enrollment in clinical trials, obtaining informed consent, managing patient care according to study protocols, collecting clinical data, monitoring for adverse events, and ensuring adherence to regulatory guidelines. Their clinical expertise is crucial for patient safety and data integrity. Many research institutions and pharmaceutical companies actively seek nurses for these roles.
For nurses interested in leading their own research or pursuing more advanced research roles, further education is often beneficial. A Master of Science in Nursing (MSN) with a research focus, a Doctor of Nursing Practice (DNP) with a project focused on evidence-based practice in cardiology, or a Ph.D. in nursing or a related biomedical science can provide the necessary training in research methodology, grant writing, and statistical analysis. Some nurses may also pursue Master's degrees in Clinical Research or Public Health. With advanced qualifications, nurses can become principal investigators, co-investigators, or research scientists, contributing to the design and execution of cardiovascular studies and the dissemination of findings. The combination of clinical nursing experience and research training creates a unique and valuable skill set.
This book provides foundational knowledge for cardiac nurses, which can be a strong base for transitioning into research focusing on similar patient populations or conditions.
What industries beyond healthcare hire CVD specialists?
While traditional healthcare settings like hospitals and clinics are primary employers, specialists with expertise in cardiovascular disease are also sought after in a variety of other industries. The pharmaceutical and biotechnology industries are major employers. Cardiologists, cardiovascular researchers (Ph.D.s), and experienced clinical trial professionals are needed for drug discovery, development, clinical trial design and management, medical affairs, and regulatory submissions for new cardiovascular therapies. Their expertise is crucial in bringing new medications from the lab to the patient.
The medical device industry is another significant sector. Companies that design, manufacture, and market devices used in cardiovascular care – such as stents, pacemakers, implantable defibrillators, artificial heart valves, and advanced imaging equipment – require the expertise of cardiovascular specialists. Roles can include research and development, clinical affairs (managing trials for new devices), medical education, sales, and marketing support. Engineers with a biomedical focus, clinicians, and scientists all play roles here.
Other industries include health insurance companies, where CVD specialists might work in medical underwriting, case management, or developing disease management programs. Legal firms may consult with cardiovascular experts for medical malpractice cases or product liability litigation. Investment firms and financial analysts covering the healthcare sector often seek insights from CVD specialists to evaluate pharmaceutical and medical device companies. Furthermore, with the rise of digital health, technology companies developing wearable devices, health apps, or AI-driven diagnostic tools are increasingly hiring individuals with cardiovascular expertise to inform product development and ensure clinical relevance. Opportunities also exist in academia (beyond clinical roles), government health agencies, and non-profit advocacy organizations.
How does automation threaten/boost CVD-related jobs?
Automation, including artificial intelligence (AI) and robotics, is poised to have a dual impact on cardiovascular disease-related jobs, presenting both potential threats and significant opportunities for boosting efficiency and creating new roles. On one hand, certain tasks currently performed by humans may become automated. For example, AI algorithms are becoming increasingly proficient at analyzing medical images (like echocardiograms or CT scans), potentially reducing the time technicians or radiologists spend on initial interpretations. AI could also automate aspects of data entry, scheduling, or routine monitoring, which might affect administrative and some clinical support roles.
However, automation is more likely to transform jobs rather than eliminate them entirely, and it will also create new job opportunities. AI can serve as a powerful assistant to clinicians, helping them to diagnose diseases earlier and more accurately, personalize treatment plans, and predict patient outcomes. This allows healthcare professionals to focus on more complex decision-making, patient interaction, and aspects of care that require human empathy and judgment. For instance, while AI might flag an abnormal ECG, a cardiologist will still be needed to interpret the findings in the context of the patient's overall clinical picture and discuss treatment options.
Furthermore, the development, implementation, and maintenance of these new automated systems will require a skilled workforce. There will be increased demand for data scientists, AI specialists with healthcare knowledge, biomedical engineers who can design and integrate these technologies, and healthcare informaticians. Clinical staff will need training to use these new tools effectively. Automation can also boost jobs by enabling new capabilities, such as remote patient monitoring on a larger scale or more sophisticated data analysis for research, leading to new roles focused on managing and interpreting these data streams. The key will be for professionals in the CVD field to adapt, acquire new skills, and embrace these technological advancements as tools to enhance, rather than replace, human expertise.
Is international experience beneficial in this field?
Yes, international experience can be highly beneficial for professionals in the cardiovascular field, offering a range of advantages for personal and career development. Working or training in a different country exposes individuals to diverse healthcare systems, patient populations, and approaches to cardiovascular care and research. This can broaden one's clinical skills, cultural competence, and understanding of global health challenges related to CVD.
For clinicians, international experience might involve participating in medical missions, undertaking a fellowship or observership abroad, or working in a healthcare system with different resources and common pathologies. This can provide unique insights into managing diseases that may be less common in their home country or learning innovative techniques. For researchers, international collaborations are often essential for conducting large-scale epidemiological studies, accessing diverse genetic data, or participating in multi-center clinical trials. Such collaborations can enhance the impact and generalizability of research findings.
Beyond the technical skills, international experience fosters adaptability, resilience, and cross-cultural communication abilities – qualities that are increasingly valued in a globalized world. It can also expand professional networks and open doors to new career opportunities. For those interested in global public health or working for international organizations like the WHO, firsthand experience in different cultural and healthcare settings is often a prerequisite. While not always a formal requirement for all career paths, seeking out international opportunities can provide a richer, more nuanced perspective on cardiovascular disease and its management, ultimately making one a more well-rounded and impactful professional in the field.
These courses can provide a starting point for understanding global health issues and disease patterns, which is relevant for anyone considering international work in cardiovascular health.
Useful Links and Resources
To further your exploration of cardiovascular disease, whether for academic, professional, or personal interest, the following resources may be helpful. These include links to major health organizations and specific OpenCourser browse pages.
Health Organizations and Information
World Health Organization (WHO) - Cardiovascular Diseases: Comprehensive information on global CVD burden, risk factors, prevention, and WHO initiatives.
U.S. Centers for Disease Control and Prevention (CDC) - Heart Disease: Data, facts, and resources on heart disease in the United States.
American Heart Association (AHA): A leading voluntary organization dedicated to fighting heart disease and stroke, offering extensive patient and professional resources.
National Heart, Lung, and Blood Institute (NHLBI): Part of the U.S. National Institutes of Health, providing research information and patient education on heart and vascular diseases.
OpenCourser Resources
Health & Medicine on OpenCourser: Browse a wide array of courses related to health, medicine, and specific conditions including cardiovascular topics.
Biology on OpenCourser: Explore foundational biology courses that underpin the understanding of human physiology and disease.
Search for "Cardiology" on OpenCourser: Find specific courses and resources related to cardiology and cardiovascular disease.
OpenCourser Learner's Guide: Discover tips and strategies for making the most of online learning, creating study plans, and integrating online courses into your educational journey.
This article has aimed to provide a thorough introduction to the multifaceted topic of cardiovascular disease, from its fundamental nature and global impact to educational pathways, career opportunities, and the latest innovations. The study and management of CVD is a challenging yet profoundly rewarding field, offering numerous avenues to contribute to human health and well-being. Whether you are just beginning to explore this area or are looking to deepen your existing knowledge, we hope this guide has equipped you with valuable insights to inform your path forward. The journey of learning is continuous, and the resources available, including those on OpenCourser, can support you every step of the way.