Medical Physicist
Medical Physicist: A Comprehensive Career Guide
Medical physics is a specialized field where the principles of physics meet the practice of medicine. It involves applying physics concepts and techniques to help diagnose and treat human diseases. Medical physicists play a vital role in healthcare, ensuring the safe and effective use of technologies like radiation therapy and medical imaging.
This career path offers intellectually stimulating challenges, combining rigorous scientific understanding with direct applications in patient care. Professionals in this field often work at the cutting edge of technology, contributing to advancements in areas like cancer treatment and diagnostic imaging. They collaborate closely with physicians and other healthcare professionals, making a tangible impact on patient outcomes.
Overview of Medical Physics
What is Medical Physics?
Medical physics is fundamentally an interdisciplinary science. It bridges the gap between the abstract world of physics and the practical, human-centered world of medicine. Professionals in this field use their deep understanding of physics principles—such as radiation, electromagnetism, and acoustics—to develop and implement medical technologies.
The core aim is to improve patient care through physics-based methods. This could involve ensuring the accuracy of a radiation dose delivered to a tumor or optimizing the quality of an MRI scan. Medical physicists are essential members of the healthcare team, providing expertise that clinicians rely on for safe and effective treatments.
The field is constantly evolving, driven by technological advancements and new discoveries in both physics and biology. This dynamic nature requires medical physicists to be lifelong learners, continuously updating their knowledge and skills.
Core Domains of Medical Physics
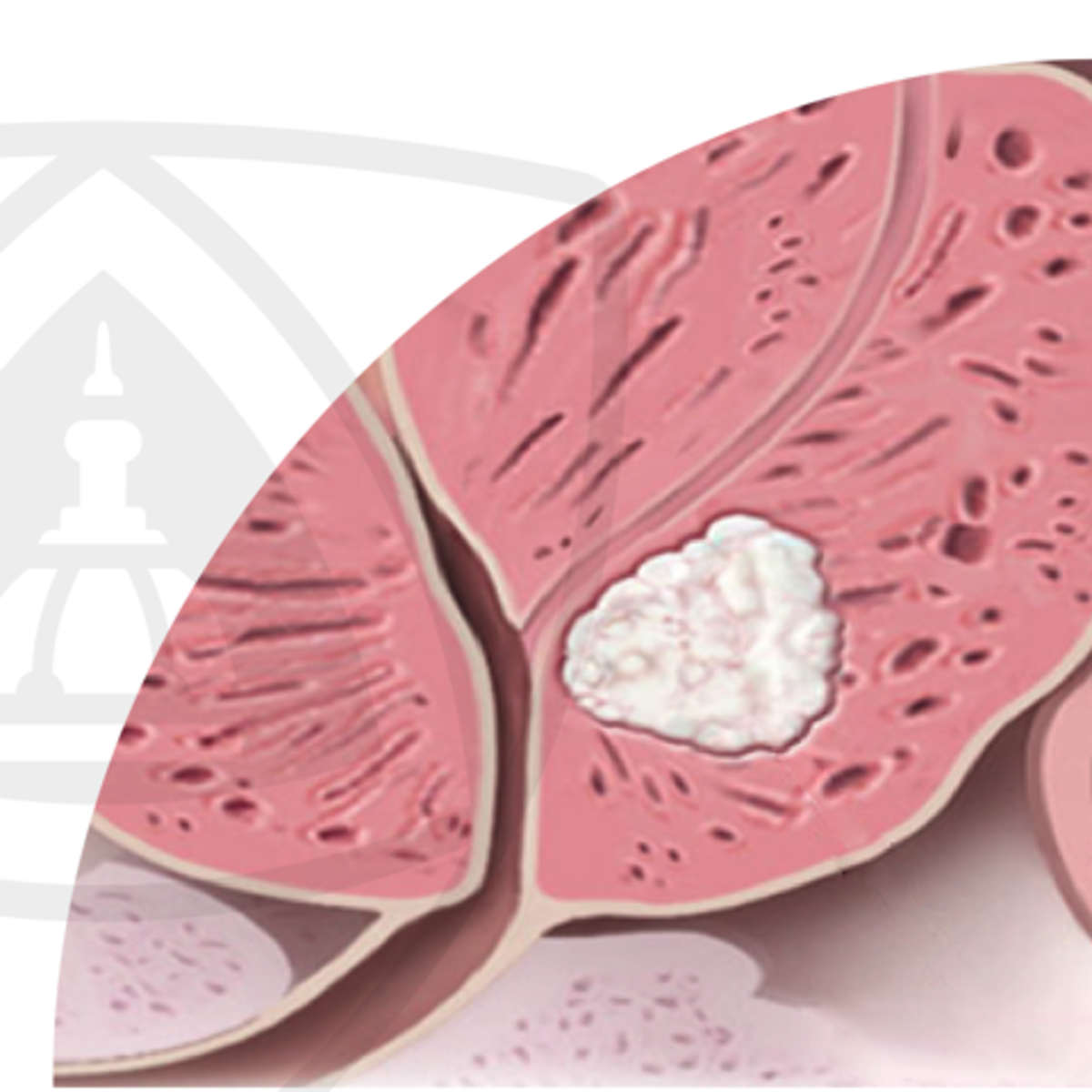
Medical physics encompasses several key areas. One major domain is radiation therapy physics, which focuses on using ionizing radiation to treat cancer and other diseases. Physicists in this area design treatment plans, ensure accurate dose delivery, and maintain the safety of radiation-producing equipment like linear accelerators.
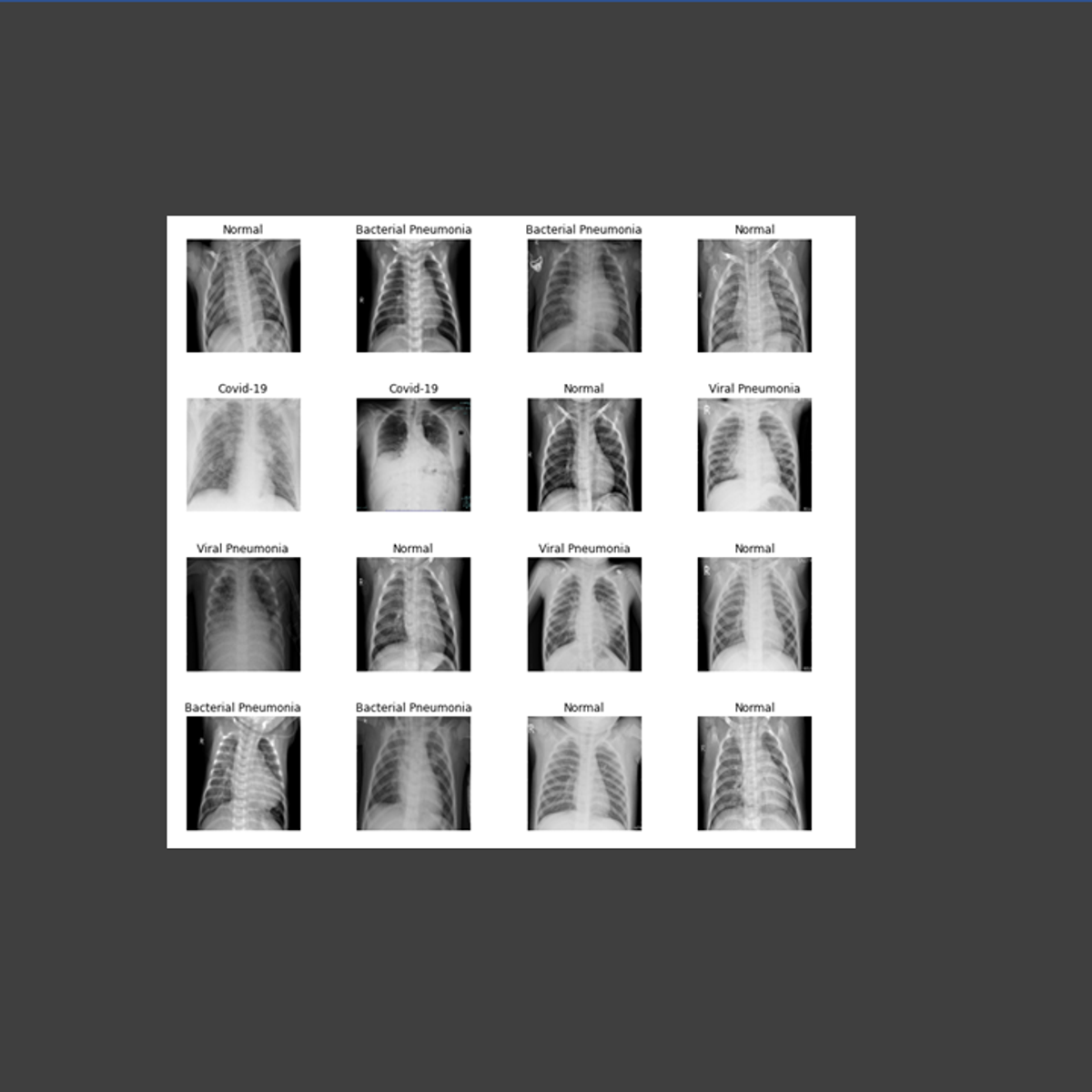
Another core domain is diagnostic imaging physics. This involves the physics principles behind imaging technologies such as X-ray, computed tomography (CT), magnetic resonance imaging (MRI), and ultrasound. Medical physicists ensure these systems produce high-quality images for accurate diagnosis while minimizing patient radiation exposure.
Nuclear medicine physics is a third domain, dealing with the use of radioactive materials (radiopharmaceuticals) for diagnosis and treatment. Physicists here are involved in dose calculation, imaging techniques like PET and SPECT, and radiation safety related to these radioactive substances.
These books offer comprehensive insights into the physics principles underlying radiation therapy and medical imaging.
Bridging Physics and Clinical Applications
Medical physicists act as crucial translators, applying complex physics principles to solve real-world clinical problems. They ensure that sophisticated medical equipment functions correctly and safely, translating technical specifications into practical clinical protocols.
Their work directly impacts patient safety and treatment effectiveness. For example, precise calibration of a radiotherapy machine is critical to delivering the intended radiation dose, minimizing harm to healthy tissue while maximizing the effect on the tumor. Similarly, optimizing MRI protocols enhances image quality, aiding physicians in making accurate diagnoses.
This bridge role requires strong communication skills alongside technical expertise. Medical physicists must effectively explain complex physics concepts to doctors, technicians, and sometimes patients, ensuring everyone understands the procedures and safety measures involved.
Global and National Regulatory Frameworks
The practice of medical physics is guided by strict regulations and standards to ensure patient and staff safety. International organizations like the International Atomic Energy Agency (IAEA) provide foundational safety standards and guidance for the medical use of ionizing radiation.
National regulatory bodies in each country implement and enforce specific requirements. In the United States, organizations like the Nuclear Regulatory Commission (NRC) and state health departments oversee the use of radioactive materials and radiation-producing machines. Professional bodies also play a role in setting standards of practice.
Compliance with these frameworks is a core responsibility for medical physicists. They are often tasked with developing and managing radiation safety programs within healthcare facilities, ensuring adherence to all applicable laws and guidelines.
These resources delve deeper into radiation safety standards and practices, which are fundamental to the field.
Roles and Responsibilities of a Medical Physicist
Radiation Safety and Quality Assurance
A primary responsibility of medical physicists is ensuring radiation safety for patients, staff, and the public. This involves developing safety protocols, monitoring radiation levels, and managing radioactive materials according to regulatory standards.
Quality assurance (QA) is another critical function. Medical physicists perform regular checks and calibrations on complex medical equipment, such as linear accelerators, CT scanners, and MRI machines, to ensure they operate accurately and safely. This meticulous QA work guarantees that diagnostic images are clear and radiation treatments are delivered precisely as prescribed.
They investigate any equipment malfunctions or incidents involving radiation, implementing corrective actions to prevent recurrence. This dedication to safety and quality underpins the trust placed in medical imaging and radiation therapy procedures.
These courses provide foundational knowledge in physics relevant to radiation and imaging principles.
Treatment Planning and System Optimization
In radiation oncology, medical physicists work closely with radiation oncologists to design individualized treatment plans for cancer patients. Using sophisticated software, they calculate the precise radiation dose distribution required to target tumors while sparing surrounding healthy tissues.
This involves complex modeling of radiation beams and patient anatomy, often using advanced imaging data like CT and MRI scans. They optimize treatment parameters, such as beam angles and intensities, to achieve the desired therapeutic outcome.
Medical physicists are also responsible for commissioning and optimizing treatment planning systems. They ensure the software accurately calculates dose distributions and integrates seamlessly with treatment delivery machines, verifying its performance before clinical use.
Equipment Calibration and Dosimetry
Accurate measurement of radiation dose (dosimetry) is fundamental to medical physics. Physicists use specialized instruments called dosimeters to measure the output of radiation-producing equipment and ensure its accuracy.
Regular calibration of equipment like linear accelerators, X-ray machines, and brachytherapy sources is essential. This process verifies that the machine delivers the correct amount of radiation, according to established standards and the treatment plan.
They maintain detailed records of all calibrations and quality assurance checks, ensuring compliance with regulatory requirements. This meticulous attention to detail is crucial for patient safety and treatment efficacy.
Understanding the underlying technology, like particle accelerators used in therapy, is beneficial.
Research and Collaboration
Many medical physicists engage in research to advance the field. This might involve developing new imaging techniques, improving radiation therapy methods, or investigating the biological effects of radiation.
Collaboration is key. Medical physicists often work alongside physicians, biologists, engineers, and computer scientists on research projects. They might contribute their expertise in physics principles, data analysis, or technology development.
Research can occur in academic institutions, hospitals, or industry settings. The goal is often to translate new scientific findings or technological innovations into improved clinical practice, ultimately benefiting patients.
Formal Education Pathways
Undergraduate Prerequisites
A strong foundation in physics is essential for aspiring medical physicists. Typically, this begins with a bachelor's degree in physics. Coursework should include classical mechanics, electromagnetism, thermodynamics, quantum mechanics, and modern physics.
Solid mathematical skills are equally crucial. Students should pursue courses in calculus (single and multivariable), differential equations, linear algebra, and potentially computational methods. A background in biology and chemistry is also highly beneficial, providing context for medical applications.
While a physics major is common, degrees in related engineering fields or other physical sciences can also serve as a foundation, provided the student completes coursework equivalent to a physics minor, including several upper-level physics courses.
These courses cover fundamental physics and chemistry concepts often required at the undergraduate level.
Graduate Programs and CAMPEP Accreditation
To practice clinically in the United States and Canada, medical physicists generally need a graduate degree (Master's or PhD) from a program accredited by the Commission on Accreditation of Medical Physics Education Programs (CAMPEP). CAMPEP ensures that programs meet rigorous standards for curriculum and training.
These graduate programs provide specialized coursework in areas like radiation physics, dosimetry, radiobiology, medical imaging physics, anatomy and physiology, and radiation safety. They combine theoretical knowledge with practical laboratory experience.
Some individuals with a PhD in physics or a related field might pursue a CAMPEP-accredited certificate program to fulfill the required didactic coursework before entering a residency.
These courses delve into areas like cancer biology and imaging, relevant to graduate-level study.
Residency Requirements and Board Certification
Following graduate studies, aspiring clinical medical physicists must complete a CAMPEP-accredited residency program. These are typically two-year, hands-on training programs in a clinical setting, providing supervised experience in areas like radiation therapy or diagnostic imaging.
Residency training is essential for developing the practical skills and clinical judgment needed to practice independently. Acceptance into residency programs is competitive and usually requires graduation from a CAMPEP-accredited graduate or certificate program.
After completing residency, physicists can pursue board certification, commonly through the American Board of Radiology (ABR) in the U.S. or the Canadian College of Physicists in Medicine (CCPM). Certification involves passing a series of rigorous exams and demonstrates a high level of competence in a specific specialty (therapeutic, diagnostic, or nuclear medical physics).
PhD Trajectories for Research-Focused Roles
While a Master's degree plus residency is sufficient for many clinical roles, a PhD is often preferred for those aiming for careers heavily focused on research and academia. A PhD program involves deeper theoretical study and culminates in original research contributing new knowledge to the field.
PhD graduates may pursue postdoctoral research positions to further specialize and build their research portfolio before seeking faculty positions at universities or research roles in national laboratories or industry.
Even within clinical settings, a PhD can open doors to leadership positions, greater involvement in research activities alongside clinical duties, and teaching responsibilities for graduate students and residents.
These books are standard references in radiation therapy physics, often used in graduate programs and by practicing physicists.
Online Learning and Skill Development
Supplemental Online Courses
Online courses can be valuable tools for supplementing formal education in medical physics. They offer flexibility for learning specialized topics or refreshing foundational knowledge. Platforms like OpenCourser catalog numerous courses relevant to physics, biology, and data analysis.
Topics like radiation biology, advanced imaging techniques, or programming skills needed for data analysis can be explored through online modules. These can be particularly helpful for students preparing for graduate studies or professionals seeking continuing education.
However, it is crucial to understand that online courses cannot replace the formal CAMPEP-accredited graduate degree and residency required for clinical practice. They serve best as supplementary resources, not alternative pathways to certification.
These online courses cover specific areas like cancer biology, imaging fundamentals, and related physics concepts, useful for supplemental learning.
Virtual Labs and Software Skills
Some online platforms may offer virtual laboratory experiences or training modules for software commonly used in medical physics, such as treatment planning systems or image analysis tools. These can provide preliminary exposure to the tools of the trade.
Developing proficiency in specific software is often part of formal residency training. Online tutorials or courses can offer an introduction, potentially helping learners become familiar with interfaces and basic functions before encountering them in a clinical or research setting.
Skills in programming languages like Python or MATLAB are also increasingly valuable for data analysis, modeling, and research in medical physics. Online courses provide accessible avenues for acquiring these computational skills.
These courses provide introductions to relevant imaging modalities and computational techniques.
Open-Source Tools and Independent Projects
The medical physics community sometimes utilizes open-source software for research and educational purposes. Engaging with these tools can be a way for self-directed learners to practice applying physics principles to simulated medical scenarios.
Independent projects, perhaps analyzing publicly available medical imaging datasets or exploring dosimetry calculations with open-source code, can deepen understanding. However, these activities lack the structured feedback and clinical context provided by formal training.
While valuable for personal development and exploration, such projects do not substitute for the experience gained through accredited programs and supervised clinical practice. They are best viewed as ways to explore interest in the field or build supplementary skills.
Integrating Online Study with Clinical Exposure
For those exploring the field or in the early stages of education, combining online learning with efforts to gain real-world exposure can be beneficial. Shadowing a medical physicist or volunteering in a related hospital department (if possible) can provide valuable context for theoretical knowledge gained online.
This integration helps bridge the gap between abstract concepts learned online and their practical application in a clinical environment. It can solidify understanding and help individuals make informed decisions about pursuing the rigorous formal pathway.
Remember, the path to becoming a practicing clinical medical physicist is structured and demanding. Use online resources strategically to support your journey through accredited education and training. The OpenCourser Learner's Guide offers tips on structuring self-study and maximizing online learning.
These courses cover advanced imaging topics and the application of AI in medicine.
Career Progression in Medical Physics
Entry-Level Roles
Upon completing a CAMPEP-accredited residency and achieving board eligibility or certification, individuals typically start in roles often titled Junior Medical Physicist or Staff Physicist. These positions involve performing routine clinical duties under the guidance of more experienced colleagues.
Responsibilities at this stage often include quality assurance testing of equipment, assisting with treatment planning, performing dose calculations, and participating in radiation safety procedures. It's a period of consolidating clinical skills and gaining practical experience.
Working in a hospital or cancer center is common for entry-level clinical physicists. The focus is on applying the knowledge and skills gained during education and residency to real patient care scenarios.
Mid-Career and Specialization
With several years of experience, medical physicists often develop deeper expertise and may choose to specialize within a subfield. Specializations can include areas like stereotactic radiosurgery (SRS/SBRT), brachytherapy (internal radiation therapy), MRI physics, or specific imaging modalities.
Mid-career physicists take on more complex tasks, may lead specific projects or quality assurance programs, and contribute to developing new clinical procedures. They often serve as mentors for residents and junior physicists.
Opportunities for advancement might involve becoming a lead physicist for a specific technology or treatment modality, or taking on roles with increased responsibility for clinical operations or safety programs.
These books cover specialized areas like gynecologic oncology and advanced radiation techniques.
Leadership Roles
Experienced medical physicists with strong leadership and management skills can advance to senior positions. Roles like Senior Medical Physicist, Lead Physicist, or Chief Medical Physicist involve overseeing physics services within a department or institution.
Responsibilities often include managing staff physicists and dosimetrists, budget planning, strategic development of physics services, ensuring regulatory compliance, and representing the physics group in institutional committees.
These leadership roles require not only deep technical expertise but also excellent communication, organizational, and interpersonal skills to manage teams and collaborate effectively with hospital administration and clinical leaders.
Alternative Paths: Industry and Academia
Beyond clinical practice in hospitals, medical physicists have career options in industry and academia. Industry roles often involve research and development for medical equipment manufacturers, working on designing, testing, or supporting new technologies like imaging scanners or treatment machines.
Other industry roles include technical sales, application support (training users on equipment), or consulting. These positions leverage physics expertise in a commercial environment.
Academic careers typically involve a combination of teaching, research, and sometimes clinical service within a university hospital setting. This path usually requires a PhD and involves mentoring students, securing research grants, and publishing scientific papers.
Industry Applications and Work Environments
Hospitals vs. Research Institutions
The most common work environment for clinical medical physicists is a hospital or dedicated cancer center. Here, the focus is primarily on direct patient care, including treatment planning, quality assurance, and radiation safety related to clinical procedures.
Medical physicists may also work in university medical centers or research institutions. While clinical duties might still be part of the role, there is often a greater emphasis on research activities, teaching medical students or residents, and developing novel techniques or technologies.
The day-to-day balance between clinical service, research, and teaching can vary significantly depending on the specific institution and the physicist's role within it.
These courses explore cancer biology and treatment concepts central to hospital and research settings.
Equipment Manufacturing Roles
Medical equipment manufacturers employ physicists in various capacities. Roles in research and development (R&D) involve designing and improving technologies like linear accelerators, MRI scanners, CT systems, and treatment planning software.
Physicists in manufacturing may also work in quality control, ensuring products meet design specifications and regulatory standards. Others might serve as application specialists, providing technical expertise and training to customers (hospitals and clinics) who purchase the equipment.
These roles offer an opportunity to work at the forefront of technological innovation, contributing to the tools used in clinical practice worldwide. A strong physics background combined with an understanding of clinical needs is valuable.
Understanding advanced imaging modalities is crucial for roles in equipment manufacturing.
Government and Regulatory Positions
Government agencies and regulatory bodies employ medical physicists to help develop and enforce safety standards related to medical radiation use. This could involve working for national organizations like the NRC or FDA in the U.S., or international bodies like the IAEA.
Responsibilities might include reviewing license applications for facilities using radiation, inspecting clinics for compliance with safety regulations, contributing to the development of new guidelines, or advising policymakers on issues related to radiation safety and medical technology.
These roles require a deep understanding of physics, radiation safety principles, and the regulatory landscape. They offer a chance to impact public health and safety on a broad scale.
Startups and AI-Driven Technologies
The rise of artificial intelligence (AI) and machine learning (ML) is creating new opportunities in medical physics, particularly within startups focused on healthcare technology. Physicists with computational skills are involved in developing AI algorithms for tasks like automated treatment planning, image analysis, and quality assurance.
These roles often blend traditional physics expertise with skills in Data Science and software development. Startups offer dynamic environments where physicists can contribute to cutting-edge innovations aiming to make medical procedures more efficient, accurate, and personalized.
These courses introduce AI concepts and their application in medical imaging, relevant for roles in startups and tech development.
Ethical and Safety Challenges
Risk Mitigation in Radiation Oncology
While radiation therapy is a powerful tool against cancer, it also carries risks. A key ethical and safety challenge is minimizing radiation dose to healthy tissues while effectively treating the tumor. Medical physicists play a central role in this balancing act through careful treatment planning and precise delivery.
Ensuring the accuracy of dose calculations and machine performance is paramount. Errors can lead to under-dosing the tumor (reducing treatment effectiveness) or over-dosing healthy organs (causing serious side effects). Rigorous quality assurance programs managed by physicists are essential for risk mitigation.
Communicating risks and benefits to patients is also important, although primarily the physician's role. Physicists provide the technical data and quality checks that support safe and effective treatment delivery.
Ethical Dilemmas in Experimental Therapies
Medical physicists involved in research may encounter ethical dilemmas related to experimental therapies or new technologies. This could involve studies testing novel radiation techniques or imaging agents where the long-term risks and benefits are not yet fully known.
Ensuring patient safety during clinical trials is a primary concern. Physicists contribute by accurately characterizing the physical aspects of the new therapy, developing safety protocols, and monitoring treatments closely.
Ethical considerations include informed consent (ensuring patients understand the experimental nature and potential risks) and equitable access to potentially beneficial new treatments. Physicists participate in institutional review board (IRB) processes that oversee research ethics.
Patient Data Privacy in AI Applications
The increasing use of AI in medical physics introduces new challenges related to patient data privacy and security. Training AI algorithms often requires large datasets of patient images and clinical information, which must be handled securely and ethically.
Medical physicists working with AI must be knowledgeable about data privacy regulations (like HIPAA in the U.S.) and employ techniques like data anonymization or federated learning to protect patient confidentiality.
Ensuring the fairness and lack of bias in AI algorithms is another ethical consideration. Algorithms trained on limited or skewed data could potentially perpetuate health disparities if not carefully developed and validated.
International Safety Standard Disparities
While organizations like the IAEA promote international safety standards, the actual implementation and regulatory enforcement can vary significantly between countries. This can create challenges, particularly for physicists working in international collaborations or in regions with less developed regulatory infrastructure.
Ensuring a consistent level of safety and quality care across different settings can be difficult. Physicists may need to adapt practices based on local resources and regulations while striving to adhere to internationally recognized best practices.
Promoting global harmonization of safety standards and supporting capacity building in lower-resource settings are ongoing efforts within the international medical physics community.
Emerging Trends in Medical Physics
FLASH Radiotherapy and Advanced Techniques
One exciting area of research is FLASH radiotherapy, which involves delivering radiation doses at ultra-high rates. Early studies suggest this might significantly reduce damage to normal tissues compared to conventional dose rates, potentially allowing for higher, more effective tumor doses.
Medical physicists are heavily involved in researching the underlying mechanisms, developing the technology needed to deliver FLASH doses accurately, and designing methods for reliable dosimetry at these extreme rates.
Other advanced techniques continually emerge, such as particle therapy (using protons or heavier ions) and novel brachytherapy approaches. Physicists are essential for understanding the complex physics of these modalities and translating them safely into clinical practice.
AI and Machine Learning in Adaptive Therapy
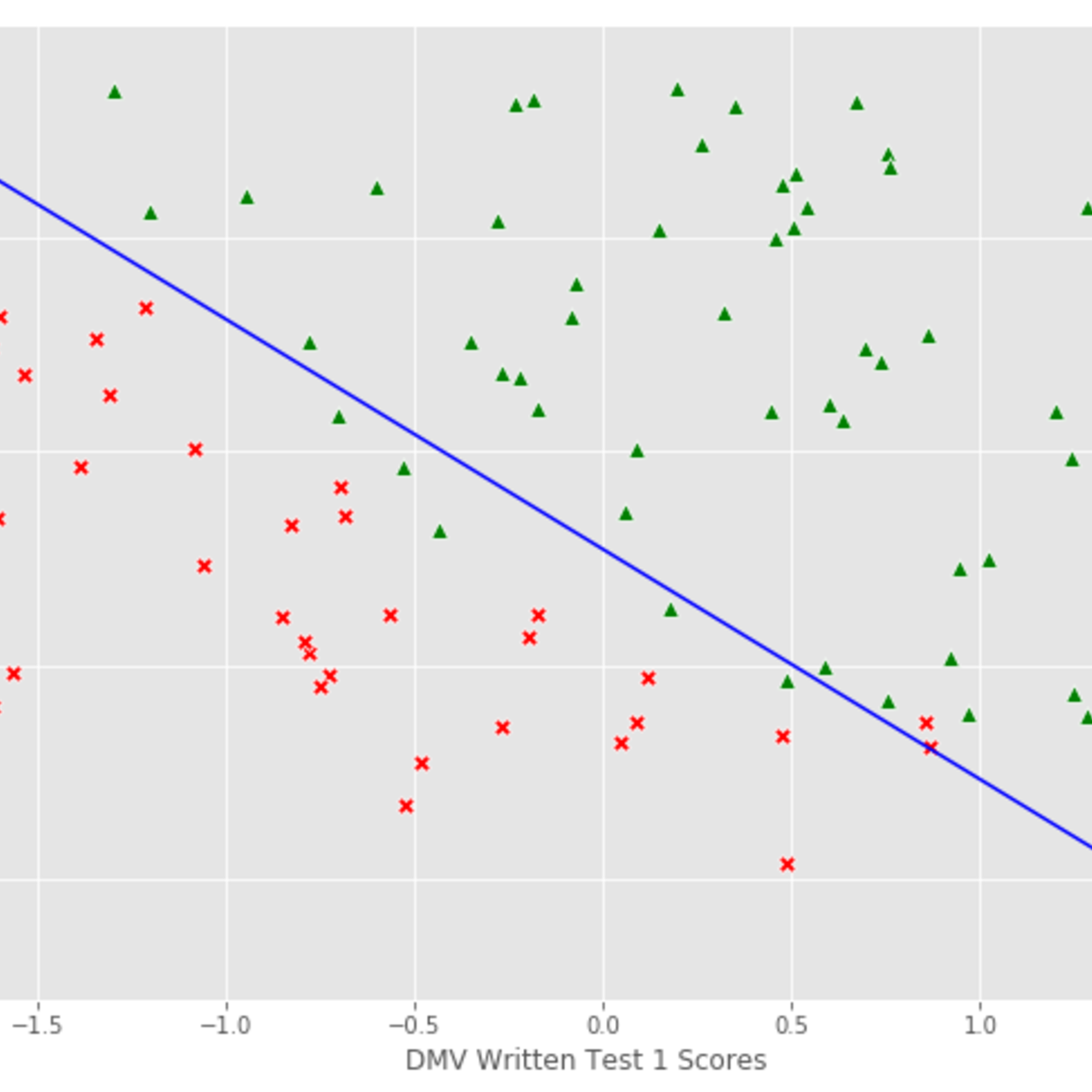
Artificial intelligence (AI) and machine learning (ML) are rapidly transforming aspects of medical physics. AI is increasingly used for tasks like automated contouring of organs on medical images, which speeds up the treatment planning process.
AI is also crucial for adaptive radiotherapy, where treatment plans are adjusted during the course of therapy based on changes in patient anatomy or tumor size observed on daily imaging. AI algorithms help automate the rapid replanning needed for these adaptive strategies, making personalized treatment more feasible.
Research continues to explore AI for predicting treatment outcomes, optimizing dose distributions automatically, and improving the quality and efficiency of various clinical workflows. As highlighted in recent studies, AI is moving from research labs into clinical practice, particularly in radiotherapy planning and image analysis.
These courses explore AI applications in medical contexts, reflecting current trends.
Globalization and Technology Access
There is a growing global demand for advanced cancer care technologies, including radiotherapy and diagnostic imaging. This presents opportunities and challenges related to making these technologies accessible and safely implemented in diverse healthcare settings worldwide.
Medical physicists play a role in international collaborations, training programs, and initiatives aimed at building capacity for medical physics practice in low- and middle-income countries. Ensuring safe and effective use of complex technologies requires adequate local expertise.
Telemedicine and remote support models, potentially leveraging cloud computing and AI, may also play a role in extending the reach of medical physics expertise globally.
Sustainability in Medical Imaging
Increasing attention is being paid to the environmental impact of healthcare, including medical imaging. High-energy equipment like MRI scanners consumes significant amounts of electricity and resources (e.g., helium for superconducting magnets).
Medical physicists may become involved in efforts to improve the energy efficiency of medical devices, optimize imaging protocols to reduce scan times or unnecessary procedures, and consider the lifecycle environmental impact of equipment.
Research into "greener" imaging technologies and sustainable practices within radiology and radiotherapy departments is an emerging area where physics expertise can contribute.
Frequently Asked Questions (Career Focus)
What are typical salary ranges?
Salaries for medical physicists vary based on experience, qualifications (e.g., board certification), geographic location, and type of employer (academic, hospital, industry). Entry-level positions typically offer competitive salaries reflecting the advanced education required.
According to data from sources like the American Physical Society and Salary.com, starting salaries for physicists with residency training might range roughly from $80,000 to $130,000 USD annually. Mid-career, board-certified physicists often earn significantly more, potentially in the $180,000 to $250,000+ range, with senior or chief physicist roles commanding even higher compensation, sometimes exceeding $280,000.
These figures are estimates and can fluctuate. Geographic location plays a significant role, with higher cost-of-living areas often correlating with higher salaries.
Is the job market saturated?
The job market for medical physicists is generally considered stable, though demand can fluctuate based on region and specialty. The need for medical physics services continues as populations age and cancer incidence rises, driving demand for radiotherapy and advanced imaging.
According to the U.S. Bureau of Labor Statistics (BLS), the overall field for physicists is projected to grow, although specific data for the medical physics subfield isn't always isolated. Some sources suggest moderate growth, driven partly by retirements and investments in areas like nuclear medicine and oncology.
Competition for residency positions can be high due to the limited number of accredited slots. However, once certified, job prospects are generally favorable, particularly for those willing to relocate.
Can I transition from a Physics or Engineering background?
Yes, transitioning from a strong physics or related engineering background is common. The standard pathway involves obtaining the necessary graduate-level medical physics coursework, typically through a CAMPEP-accredited Master's, PhD, or certificate program.
Following the didactic coursework, completion of a CAMPEP-accredited residency is required for clinical practice. Your existing physics or engineering degree provides the essential foundation, but the specialized medical physics education and clinical training are non-negotiable steps for becoming a qualified clinical medical physicist.
This transition requires significant commitment in terms of time and education. It's a challenging but achievable path for those dedicated to applying their physics skills in a healthcare setting. Exploring relevant topics through Health & Medicine courses online can help gauge interest.
What is the work-life balance like?
Work-life balance can vary depending on the role and work environment. Clinical physicists in busy hospital settings may occasionally work evenings or weekends to handle emergencies, equipment issues, or specific treatment schedules (e.g., total body irradiation).
Standard work weeks are typically around 40 hours, but project deadlines, research commitments, or heavy clinical workloads can sometimes require longer hours. Academic positions might offer more flexibility in scheduling but often involve pressures related to grant writing and publishing.
Overall, compared to some clinical professions, medical physics can offer a relatively predictable schedule, but demands can be high, particularly during residency or in demanding clinical environments.
Are there part-time or consulting opportunities?
Yes, part-time and consulting opportunities exist, particularly for experienced, board-certified physicists. Smaller clinics or hospitals that cannot support a full-time physicist might contract for services like quality assurance, regulatory compliance, or occasional treatment planning support.
Some physicists establish independent consulting practices, offering specialized expertise to multiple clients. Consulting roles might focus on areas like radiation safety audits, shielding design for new facilities, or expert witness testimony.
Part-time clinical or academic positions may also be available, though they might be less common than full-time roles, especially early in one's career.
What about international certification reciprocity?
Certification requirements differ by country. While CAMPEP accreditation for education and residency is the standard in the U.S. and Canada, other countries have their own systems. The American Board of Radiology (ABR) certification is highly respected internationally but may not automatically grant the right to practice elsewhere.
Some countries may have pathways for recognizing foreign qualifications, potentially requiring additional exams or supervised practice. Conversely, those certified abroad seeking to practice in the U.S. or Canada generally need to meet ABR/CCPM requirements, which often involves completing a CAMPEP-accredited residency.
Investigating the specific requirements of the country where you intend to practice is essential. Professional organizations like the International Organization for Medical Physics (IOMP) can be resources for understanding global standards and practices.
Conclusion
Embarking on a career as a Medical Physicist is a commitment to a rigorous, intellectually demanding, yet deeply rewarding path. It requires a strong aptitude for physics and mathematics, coupled with a dedication to applying these skills within the complex and evolving landscape of healthcare. Medical physicists make critical contributions to patient safety and treatment effectiveness in areas like radiation therapy and diagnostic imaging, working at the intersection of science, technology, and medicine. The journey involves extensive education and specialized clinical training, but leads to diverse opportunities in hospitals, research institutions, industry, and regulatory bodies. If the challenge of bridging physics and medicine excites you, further exploration using resources like those found on OpenCourser can help illuminate your path forward in this impactful field.