Healthcare Manager
Exploring a Career as a Healthcare Manager
Healthcare managers, also known as healthcare administrators or executives, are the professionals who plan, direct, and coordinate medical and health services. They might manage an entire facility, a specific clinical area or department, or a medical practice for a group of physicians. These managers work behind the scenes to ensure healthcare facilities operate efficiently, effectively, and in compliance with complex regulations, ultimately supporting the delivery of quality patient care.
Working as a healthcare manager can be deeply rewarding. You play a critical role in shaping the healthcare experience for patients and providers alike, tackling challenges that blend business acumen with a mission-driven focus on health outcomes. The field offers diverse opportunities, from managing hospital operations to leading public health initiatives, allowing individuals to find niches that align with their skills and passions. It's a dynamic career requiring sharp analytical skills, strong leadership, and a commitment to continuous improvement within the vital healthcare sector.
What Does a Healthcare Manager Do?
Understanding the multifaceted role of a healthcare manager begins with recognizing the blend of operational oversight and strategic planning involved. These professionals ensure the smooth functioning of healthcare settings, navigating the complexities of patient care delivery, finance, and regulatory landscapes.
Defining the Scope of Healthcare Management
Healthcare management involves overseeing the operational and administrative functions of healthcare facilities or systems. This broad scope encompasses everything from managing budgets and staff to ensuring compliance with healthcare laws and improving the quality and efficiency of care delivery. Managers act as crucial links between clinical staff, administrative personnel, and governing bodies.
The work requires a unique blend of skills, including leadership, financial acumen, understanding of healthcare policy, and strong communication abilities. Managers must make informed decisions that balance patient needs, organizational goals, and resource constraints. Their goal is to create an environment where healthcare professionals can provide the best possible care.
They work in diverse settings such as hospitals, clinics, nursing homes, public health departments, and insurance companies. The specific responsibilities vary significantly depending on the size and type of the organization, but the core mission remains consistent: optimizing healthcare delivery.
Core Objectives and Goals
The primary objective of a healthcare manager is to ensure the efficient and effective delivery of healthcare services. This involves optimizing resource allocation, including staffing, finances, and equipment, to meet patient needs and organizational targets. They strive to enhance operational workflows and reduce waste.
Improving patient care quality and safety is another fundamental goal. Managers implement quality improvement initiatives, monitor performance metrics, and ensure adherence to clinical standards and best practices. They foster a culture of safety and continuous improvement within their teams and departments.
Financial health is also a key responsibility. Healthcare managers develop and oversee budgets, manage revenue cycles, and make strategic financial decisions to ensure the organization's sustainability. They must navigate the complexities of healthcare financing, including insurance reimbursement and government funding streams.
These courses offer insights into the core functions and challenges faced by healthcare managers, covering service innovation and operational aspects.
A Brief History of the Role
The field of healthcare management emerged as healthcare systems grew more complex throughout the 20th century. Early hospital administrators often came from nursing or clinical backgrounds, focusing primarily on basic operational tasks. The increasing complexity of medical technology, financing, and regulation necessitated specialized management expertise.
Formal education programs in hospital administration began appearing in the mid-20th century, professionalizing the role. The focus shifted from simple administration to strategic management, encompassing finance, policy, quality improvement, and organizational leadership. The role evolved to meet the demands of a rapidly changing healthcare landscape.
Today, healthcare management is a recognized profession requiring advanced education and specialized skills. Managers grapple with contemporary issues like electronic health records, value-based care models, population health management, and health equity, reflecting the ongoing evolution of the healthcare industry itself.
This book provides historical context on major health events that shaped modern healthcare systems.
Where Healthcare Managers Work
Healthcare managers are employed across a wide spectrum of organizations within the health sector. Hospitals are perhaps the most common setting, where managers oversee departments like surgery, nursing, finance, or information technology, or even lead the entire facility as CEOs or COOs.
Physician practices, especially larger group practices and clinics, also rely heavily on healthcare managers. In these settings, managers handle business operations, billing, scheduling, and staff management, allowing physicians to focus on patient care. They ensure the practice runs smoothly and profitably.
Other significant employers include long-term care facilities (nursing homes, assisted living), home healthcare agencies, public health departments at local, state, and federal levels, health insurance companies, and consulting firms specializing in healthcare. The diversity of settings offers varied career paths and specialization opportunities.
You can explore related careers often found in similar settings.
Roles and Responsibilities in Detail
The day-to-day work of a healthcare manager is diverse, involving a mix of operational duties, strategic planning, and leadership. Understanding these specific responsibilities provides a clearer picture of the demands and rewards of the career.
Operational vs. Strategic Duties
Operational responsibilities focus on the daily functioning of a healthcare unit or facility. This includes managing schedules, overseeing workflows, ensuring adequate supplies, handling immediate problems, and maintaining compliance with daily operational standards. It's about keeping the engine running smoothly.
Strategic responsibilities, conversely, involve long-term planning and decision-making. This includes developing departmental or organizational goals, planning for future service lines, analyzing market trends, implementing major changes like new technology adoption, and ensuring the organization's long-term viability and growth.
Effective healthcare managers must excel at both. They need to address pressing operational issues while simultaneously steering their department or organization toward future goals, requiring both tactical execution and strategic foresight.
This course delves into strategic decision-making within healthcare settings.
Managing Staff and Collaboration
Leading and managing staff is a central part of the role. This includes hiring, training, evaluating, and motivating employees, who often come from diverse professional backgrounds (clinical, administrative, technical). Managers must foster a positive work environment and address personnel issues effectively.
Interdisciplinary collaboration is crucial in healthcare. Managers facilitate communication and teamwork among different departments and professional groups, such as physicians, nurses, technicians, and administrative staff. They work to break down silos and ensure coordinated patient care.
Strong leadership and interpersonal skills are essential for building cohesive teams and navigating the complex dynamics of healthcare organizations. Managers must be adept at conflict resolution, team building, and communication to ensure everyone works towards common goals.
These resources explore leadership and team management, which are vital skills for healthcare managers.
Financial Stewardship and Budgeting
Healthcare managers bear significant responsibility for the financial health of their departments or organizations. This involves developing budgets, monitoring expenditures, managing revenue streams, and implementing cost-control measures without compromising patient care quality.
Understanding healthcare finance, including billing codes, reimbursement models (like fee-for-service vs. value-based payments), and insurance contracts, is critical. Managers must analyze financial data to make informed decisions about resource allocation and investments.
They often work closely with finance departments and must be able to communicate financial information clearly to clinical staff and other stakeholders. Financial stewardship requires balancing the mission of providing care with the need for fiscal responsibility and sustainability.
These books provide foundational knowledge in health economics and finance.
Quality Assurance and Regulatory Compliance
Ensuring high-quality patient care and safety is paramount. Healthcare managers oversee quality improvement programs, track key performance indicators (KPIs), analyze patient outcomes, and implement changes based on data and best practices. They champion a culture focused on quality.
The healthcare industry is heavily regulated. Managers must ensure their operations comply with a vast array of laws and regulations from bodies like The Joint Commission, CMS (Centers for Medicare & Medicaid Services), and state health departments. This includes areas like patient privacy (HIPAA), safety protocols, and billing practices.
Staying current with evolving regulations and quality standards is an ongoing challenge. Managers are responsible for educating staff, implementing necessary policies and procedures, and preparing for audits and inspections. Failure to comply can result in significant penalties and reputational damage.
These resources cover aspects of quality improvement and compliance in healthcare.
Educational Pathways to Become a Healthcare Manager
Embarking on a career in healthcare management typically requires specific educational qualifications. Understanding the various pathways, from undergraduate degrees to specialized certifications, can help aspiring managers plan their journey.
Undergraduate Foundations
A bachelor's degree is generally the minimum requirement for entry-level administrative or management positions in healthcare. Relevant majors include Health Administration (BHA), Health Services Management, Public Health, or Business Administration with a healthcare concentration.
Some individuals enter healthcare management after gaining clinical experience, holding degrees like a Bachelor of Science in Nursing (BSN). Clinical background combined with management education can be a significant advantage, providing a deep understanding of patient care processes.
Undergraduate programs provide foundational knowledge in healthcare systems, management principles, finance, health law, and ethics. They equip students with the basic competencies needed to start their careers in the field.
Graduate Studies: MHA, MBA, and More
For career advancement and leadership roles, a master's degree is often preferred or required. The Master of Health Administration (MHA) is a specialized degree focusing specifically on healthcare management, policy, finance, and leadership within health organizations.
Another common route is the Master of Business Administration (MBA) with a concentration in healthcare management. This degree provides broader business training applicable across industries but with a specific focus on the healthcare sector's unique challenges and opportunities.
Other relevant graduate degrees include the Master of Public Health (MPH), particularly for roles in public health agencies or community health, and Master of Science degrees in specific areas like Health Informatics or Healthcare Quality and Safety.
Online programs have made graduate education more accessible for working professionals seeking to transition into or advance within healthcare management. Platforms like OpenCourser list numerous options from reputable universities, allowing learners to compare programs and find flexible learning solutions.
These courses provide foundational knowledge often covered in MHA or related programs.
Professional Certifications
While not always mandatory, professional certifications can enhance credibility and career prospects. The Fellow of the American College of Healthcare Executives (FACHE) credential is highly respected and signifies expertise and commitment to the field. It typically requires a master's degree, healthcare management experience, continuing education, and passing an exam.
Other certifications exist for specialized areas, such as the Certified Professional in Healthcare Quality (CPHQ) or the Certified Professional in Healthcare Information and Management Systems (CPHIMS). These demonstrate proficiency in specific domains like quality improvement or health IT.
Certifications often require ongoing professional development and recertification, encouraging lifelong learning and ensuring managers stay current with industry best practices and evolving trends.
Research and Doctoral Paths
For those interested in research, academia, or high-level policy work, doctoral degrees such as a PhD in Health Services Research, Health Policy, or a Doctor of Health Administration (DHA) are available. These programs focus on advanced research methodologies, policy analysis, and contributing new knowledge to the field.
PhD programs typically prepare individuals for careers in university teaching and research or roles in research institutions and government agencies. DHA programs are often practice-oriented, designed for experienced executives seeking to deepen their expertise and leadership capabilities.
While less common than master's degrees for typical management roles, doctoral studies represent the highest level of academic achievement in the field and open doors to specialized leadership and research opportunities.
Career Progression and Opportunities
A career in healthcare management offers diverse pathways for growth, from initial entry-level positions to executive leadership roles. Understanding the typical progression and potential alternative branches can help individuals navigate their professional development.
Starting Your Career: Entry-Level Roles
Graduates typically begin in entry-level administrative or coordinating roles. Positions like Department Coordinator, Project Assistant, Administrative Fellow, or Practice Assistant provide foundational experience in healthcare operations, workflow management, and administrative tasks.
These roles offer exposure to different facets of healthcare management, such as scheduling, billing, patient relations, or supporting departmental managers. They are crucial for building practical skills and understanding the complexities of the healthcare environment firsthand.
Networking, mentorship, and demonstrating initiative in these early roles are key to identifying opportunities for advancement and specialization within the organization or the broader field.
Moving Up: Mid-Career and Director Roles
With experience and often a master's degree, healthcare managers can advance to mid-level management positions. Roles like Department Manager, Service Line Director, Practice Manager, or Nursing Home Administrator involve greater responsibility for overseeing specific functions, teams, and budgets.
These positions require stronger leadership skills, strategic thinking, and financial acumen. Managers at this level are often responsible for implementing operational improvements, managing larger teams, and contributing to organizational strategy within their specific area of oversight.
Continued professional development, perhaps through certifications like FACHE or specialized training, becomes increasingly important for demonstrating expertise and readiness for further advancement into senior leadership.
This book focuses on achieving excellence in management within healthcare settings.
Reaching the Top: Executive Leadership
Experienced and accomplished healthcare managers may progress to executive leadership roles within healthcare organizations. Titles such as Chief Operating Officer (COO), Chief Financial Officer (CFO), Chief Nursing Officer (CNO), or Chief Executive Officer (CEO) represent the pinnacle of healthcare management.
These roles involve setting the overall strategic direction, overseeing entire organizations or major divisions, managing significant budgets, representing the organization externally, and making high-stakes decisions that impact thousands of patients and employees. They require exceptional leadership, vision, and political savvy.
The path to executive leadership is demanding, often requiring decades of experience, advanced degrees, a strong track record of success, and extensive professional networks. These leaders shape the future of healthcare delivery within their organizations and communities.
Alternative Career Branches
The skills and knowledge gained in healthcare management are transferable to related fields. Experienced managers may transition into healthcare consulting, advising organizations on operational efficiency, strategy, or regulatory compliance. This offers variety and the chance to work with diverse clients.
Another path lies in health policy, working for government agencies, think tanks, or advocacy groups to shape healthcare laws and regulations. This leverages expertise in healthcare systems to influence broader systemic change.
Opportunities also exist in health information technology companies, pharmaceutical firms, medical device manufacturers, and insurance companies, where knowledge of healthcare operations and management is highly valued. These alternative branches provide diverse avenues for leveraging healthcare management expertise.
These courses touch upon policy and broader health system considerations relevant to consulting or policy roles.
Emerging Trends Shaping Healthcare Management
The healthcare landscape is constantly evolving, driven by technological advancements, policy changes, and shifting patient expectations. Healthcare managers must adapt to these trends to lead effectively and ensure their organizations remain relevant and successful.
Telehealth Integration
The rapid expansion of telehealth presents both opportunities and challenges. Managers must oversee the integration of virtual care platforms, ensure seamless workflows between in-person and remote services, and address issues related to technology access, reimbursement policies, and maintaining quality of care remotely.
Managing telehealth requires adapting staffing models, training clinicians and patients on new technologies, ensuring data privacy and security in virtual environments, and evaluating the effectiveness and patient satisfaction associated with remote consultations.
Healthcare managers play a key role in developing strategies for optimizing telehealth services, ensuring they complement traditional care models effectively and equitably, reaching diverse patient populations.
Transition to Value-Based Care
The shift from fee-for-service to value-based care models fundamentally changes how healthcare organizations are reimbursed. Instead of payment per service, reimbursement is increasingly tied to patient outcomes, quality metrics, and cost efficiency.
Managers must lead efforts to redesign care processes, improve care coordination, invest in preventive health, and utilize data analytics to track outcomes and costs. This requires a focus on population health management and collaboration across the care continuum.
Adapting to value-based care requires strong analytical skills to understand performance data, leadership to drive cultural change towards quality and efficiency, and strategic planning to navigate new payment structures and risk-sharing arrangements.
This topic and course directly address value-based care and relevant organizational models.
Artificial Intelligence (AI) in Operations
Artificial intelligence is increasingly being used in healthcare for tasks ranging from diagnostic support to operational optimization. Managers need to understand the potential applications of AI in areas like predictive staffing, patient flow optimization, supply chain management, and administrative task automation.
Implementing AI requires careful planning regarding data infrastructure, ethical considerations (bias, privacy), staff training, and integrating AI tools into existing workflows. Managers must evaluate the return on investment and ensure AI adoption genuinely improves efficiency or care quality.
Staying informed about AI advancements and their potential impact on healthcare operations is becoming crucial for strategic planning and maintaining a competitive edge in the rapidly evolving technological landscape.
Explore the intersection of AI and healthcare with this topic.
Global Health Workforce Challenges
Many regions face significant shortages of healthcare professionals, including physicians, nurses, and technicians. Healthcare managers must develop strategies for recruitment, retention, and optimizing the productivity of the existing workforce.
This involves creating attractive work environments, investing in staff development and well-being programs to combat burnout, exploring innovative staffing models (e.g., team-based care), and potentially leveraging technology to augment staff capabilities.
Addressing workforce challenges requires strategic human resource management, understanding labor market dynamics, and potentially advocating for policies that support the healthcare workforce pipeline. Managers play a vital role in ensuring adequate staffing to meet patient care demands.
This book touches upon preparedness, a key aspect when facing workforce or resource limitations.
Essential Competencies for Healthcare Managers
Success in healthcare management requires a diverse skill set, encompassing technical knowledge, analytical abilities, and crucial interpersonal skills. Developing these competencies is key for aspiring and current managers.
Technical Skills and Health IT
Proficiency with healthcare information technology (HIT) systems is essential. This includes familiarity with Electronic Health Records (EHR), billing systems, scheduling software, and data analysis tools. Managers need to understand how these systems work and how to leverage them for operational efficiency and decision-making.
Understanding data management principles, including data security and privacy regulations like HIPAA, is critical. As healthcare becomes more data-driven, managers need the technical literacy to oversee IT projects, interpret data reports, and ensure the integrity and security of patient information.
Keeping up-to-date with advancements in HIT, such as interoperability standards, telehealth platforms, and cybersecurity threats, is an ongoing requirement for effective management in the modern healthcare environment.
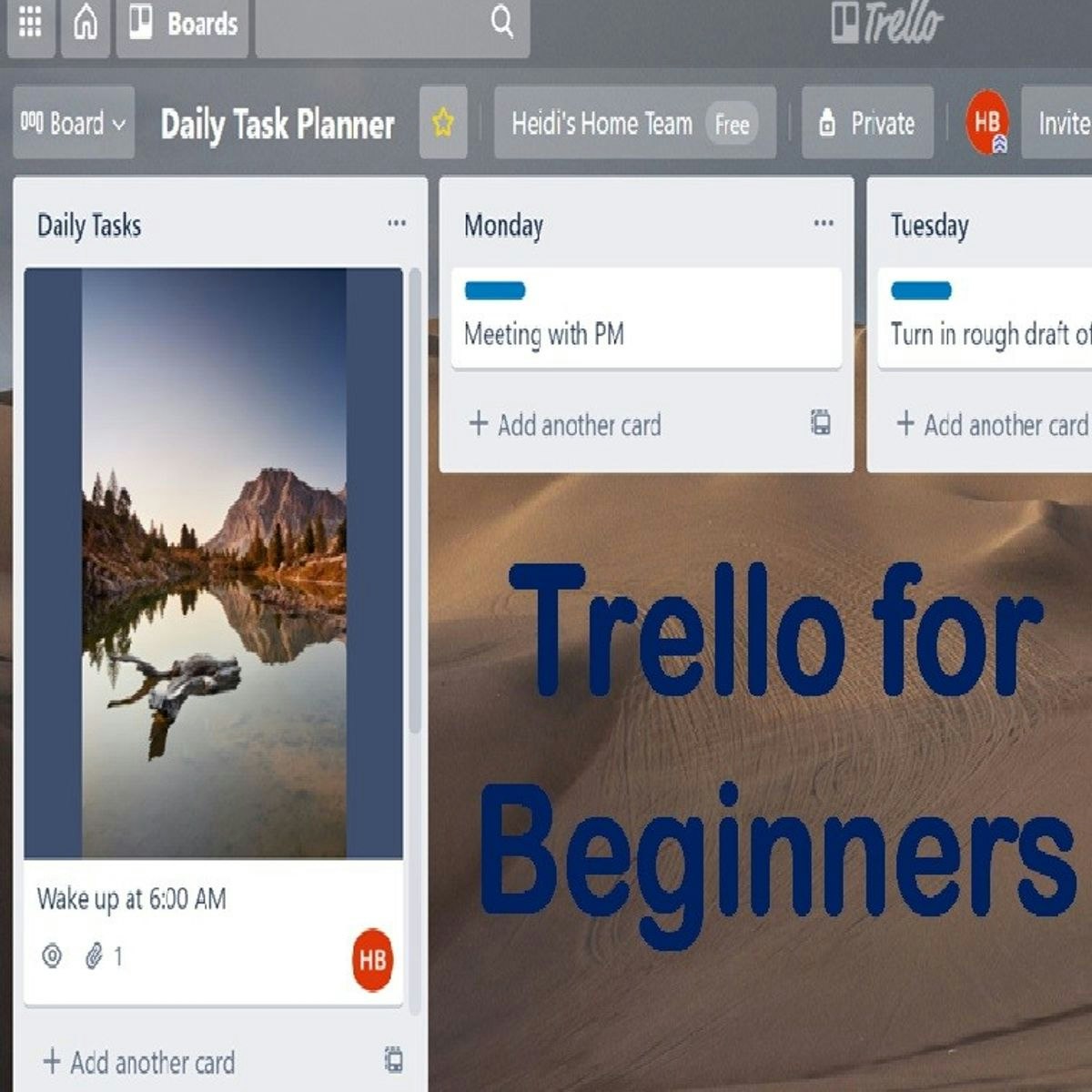
These courses cover health informatics and relevant project management tools.
Soft Skills: Communication and Leadership
Strong communication skills are paramount. Managers must effectively communicate with diverse audiences, including clinical staff, administrators, patients, and external stakeholders. This includes written, verbal, and presentation skills, as well as active listening.
Leadership abilities are crucial for guiding teams, motivating staff, managing change, and fostering a positive organizational culture. This involves skills like decision-making, problem-solving, conflict resolution, and strategic thinking.
Crisis communication is a specific soft skill vital in healthcare. Managers must be prepared to communicate clearly, calmly, and effectively during emergencies, outbreaks, or other critical incidents, managing information flow and addressing concerns from staff and the public.
Developing strong interpersonal or 'soft' skills is fundamental for navigating the human dynamics inherent in healthcare management.
Data Literacy and Analytical Skills
Healthcare managers increasingly rely on data to make informed decisions. Data literacy – the ability to read, understand, analyze, and communicate data – is a critical competency. This involves understanding key performance indicators (KPIs), statistical concepts, and data visualization techniques.
Analytical skills are needed to interpret complex datasets related to patient outcomes, operational efficiency, financial performance, and market trends. Managers must be able to identify patterns, draw meaningful conclusions, and use data to support strategic initiatives and quality improvements.
Proficiency with data analysis tools, ranging from basic spreadsheet software like Excel to more advanced business intelligence platforms like Tableau, can be highly advantageous for extracting insights from healthcare data.
These courses focus on data visualization and analysis, crucial skills for modern managers.
Cultural Competency and Patient Centricity
Healthcare organizations serve diverse patient populations. Cultural competency – understanding and respecting cultural differences in health beliefs, practices, and communication styles – is essential for providing equitable and effective care. Managers must promote cultural competency among staff and ensure services are accessible and appropriate for all patients.
A patient-centric approach places the patient's needs, values, and preferences at the center of all decisions. Managers foster this approach by designing patient-friendly processes, soliciting patient feedback, and ensuring staff are trained in empathetic communication and shared decision-making.
Developing cultural humility and maintaining a focus on the patient experience are vital for building trust, improving health outcomes, and ensuring the organization fulfills its mission of serving the community effectively.
Ethical Considerations in Healthcare Management
Healthcare managers frequently encounter complex ethical dilemmas that require careful consideration and principled decision-making. Navigating these challenges is a critical aspect of responsible leadership in the healthcare sector.
Resource Allocation Dilemmas
Decisions about how to allocate limited resources – such as staffing, beds, equipment, or funding – often involve ethical trade-offs. Managers must balance the needs of individual patients with the needs of the broader patient population and the financial sustainability of the organization.
These dilemmas can be particularly acute during public health crises or when dealing with expensive new technologies or treatments. Establishing fair, transparent criteria for resource allocation and engaging stakeholders in these difficult decisions are crucial ethical responsibilities.
Frameworks for ethical decision-making can help managers navigate these situations, ensuring choices are justifiable and align with organizational values and principles of justice and fairness.
This book explores ethical considerations, particularly regarding resource distribution.
Patient Privacy vs. Operational Needs
Protecting patient confidentiality, as mandated by laws like HIPAA, is a fundamental ethical obligation. However, operational needs, such as quality improvement initiatives, research, or efficient workflow management, often require access to patient data.
Managers must implement robust policies and technical safeguards to protect patient privacy while enabling necessary operational functions. This involves defining appropriate access levels, ensuring data anonymization or de-identification where possible, and training staff on privacy protocols.
Balancing the ethical imperative of privacy with the practical requirements of running a healthcare organization requires careful judgment and a commitment to upholding patient trust.
This book delves into public health ethics, which often involves balancing individual rights and community needs.
Mitigating Staff Burnout
Healthcare professionals often work under high stress, leading to significant rates of burnout. Managers have an ethical responsibility to create a work environment that supports staff well-being and mitigates factors contributing to burnout, such as excessive workloads, lack of control, or inadequate support.
This involves promoting work-life balance, ensuring adequate staffing levels, providing access to mental health resources, fostering a culture of respect and psychological safety, and empowering staff in decision-making processes.
Addressing burnout is not only an ethical imperative for supporting staff but also crucial for maintaining patient safety and quality of care, as burned-out staff are more prone to errors.
Conflicts of Interest
Healthcare managers may face situations involving potential conflicts of interest, where their personal interests could potentially influence their professional decisions. This might arise from relationships with vendors, personal investments, or other external affiliations.
Organizations typically have policies requiring disclosure of potential conflicts and procedures for managing them. Managers must be vigilant in identifying and disclosing such situations and recusing themselves from decisions where their objectivity could be compromised.
Maintaining transparency and prioritizing the interests of patients and the organization over personal gain is essential for upholding ethical standards and public trust.
This book specifically addresses conflicts of interest within the medical field.
Global Perspectives on Healthcare Management
Healthcare systems and management practices vary significantly around the world. Understanding these global perspectives provides valuable context and insights for managers operating in an increasingly interconnected world.
Comparing Healthcare Systems
Different countries employ diverse models for funding and delivering healthcare. Comparing systems, such as the largely private, employer-based system in the U.S. versus single-payer systems common in Canada and many European countries, highlights different approaches to access, cost, and quality.
Managers can learn from the successes and challenges of other systems. Understanding how different models address issues like universal coverage, cost containment, and health equity can inform policy debates and potential reforms within their own systems.
Studying international healthcare systems broadens a manager's understanding of the various ways healthcare can be organized and financed, fostering a more nuanced perspective on their own operating environment.
These resources offer insights into different health policies and systems.
Challenges in Developing Nations
Healthcare managers in developing nations often face unique challenges, including limited resources, inadequate infrastructure, significant workforce shortages, and a high burden of infectious diseases alongside growing rates of chronic conditions.
Management strategies in these contexts must focus on maximizing impact with scarce resources, building basic infrastructure, strengthening primary care, leveraging community health workers, and adapting solutions to local needs and cultural contexts.
International collaborations, global health initiatives, and technology (like mobile health) play important roles in supporting healthcare delivery in resource-limited settings. Managers working in or collaborating with these regions require specific skills in cross-cultural adaptation and resource optimization.
Cross-Cultural Leadership Skills
As healthcare becomes more globalized, with diverse workforces and patient populations, cross-cultural leadership skills are increasingly vital. Managers must be adept at leading teams composed of individuals from various cultural backgrounds and serving patients with diverse beliefs and expectations.
This requires cultural sensitivity, effective cross-cultural communication, an understanding of different work styles, and the ability to build inclusive environments where diversity is valued. Adapting leadership approaches to different cultural contexts is key.
For managers working in international settings or multinational organizations, these skills are essential for navigating complex intercultural dynamics and fostering effective collaboration.
Medical Tourism and Its Implications
Medical tourism, where patients travel across borders to receive medical care, presents both opportunities and challenges for healthcare managers. It can be a source of revenue but also raises ethical questions about equity and potential impacts on local healthcare access.
Managers in facilities catering to international patients must navigate issues related to marketing, international accreditation, language barriers, cultural sensitivity, continuity of care across borders, and managing legal and ethical complexities.
Understanding the drivers and implications of medical tourism is important for strategic planning, particularly for organizations located in regions that are popular destinations for international patients.
Frequently Asked Questions (FAQs)
Here are answers to some common questions individuals have when considering a career in healthcare management.
What's the difference between a Healthcare Manager and a Hospital Administrator?
The terms are often used interchangeably, but "Healthcare Manager" can be broader. While a Hospital Administrator typically focuses on managing operations within a hospital setting, a Healthcare Manager might work in various environments like clinics, nursing homes, insurance companies, or public health agencies.
Functionally, their roles are very similar, involving planning, directing, and coordinating health services. The key distinction often lies in the specific setting and scope of responsibility. Both roles require strong leadership, financial acumen, and knowledge of healthcare systems.
Think of Hospital Administrator as a specific type of Healthcare Manager focused on the hospital environment. Other healthcare managers might specialize in managing physician practices, long-term care facilities, or specific departments across various settings.
What is the typical salary range?
Salaries for healthcare managers vary widely based on factors like experience, education level, geographic location, type and size of the employing organization, and specific responsibilities. Entry-level positions might start lower, while executive roles command significantly higher compensation.
According to the U.S. Bureau of Labor Statistics (BLS), the median annual wage for medical and health services managers was $110,680 as of May 2023. However, the lowest 10 percent earned less than $67,960, and the highest 10 percent earned more than $216,750, illustrating the wide range.
Factors like holding an advanced degree (MHA, MBA) or professional certifications (FACHE) can positively influence earning potential. Salaries tend to be higher in major metropolitan areas and larger healthcare systems compared to rural areas or smaller practices.
What is the job outlook and demand?
The job outlook for healthcare managers is very positive. The BLS projects employment of medical and health services managers to grow 28 percent from 2022 to 2032, much faster than the average for all occupations.
This strong growth is driven by several factors, including the aging baby-boom population requiring more healthcare services, advancements in medical technology, and the increasing complexity of healthcare regulations and insurance systems. There is a growing need for managers to coordinate care and improve efficiency.
As the large baby-boom generation ages and people remain active later in life, the healthcare industry will likely see an increase in demand for medical services. This translates to continued demand for managers who can organize and oversee the delivery of these services effectively. Exploring courses in Health & Medicine or Management on OpenCourser can provide relevant skills.
How can I transition from a clinical role to management?
Many healthcare managers start in clinical roles (e.g., nursing, therapy, physician). Transitioning often involves pursuing further education, such as an MHA, MBA in Healthcare, or relevant certifications. Gaining administrative experience through committee work, project leadership, or supervisory roles within your clinical department is also beneficial.
Highlighting transferable skills like problem-solving, communication, teamwork, and understanding clinical workflows is crucial. Networking with current managers and seeking mentorship can provide guidance and open doors to administrative opportunities.
Making the switch requires demonstrating leadership potential and a clear interest in the business and operational aspects of healthcare. It's a common and often successful career path, as clinical experience provides valuable ground-level perspective for management roles. Consider leveraging online resources like the OpenCourser Learner's Guide for tips on structuring your learning path.
Will AI impact job security for Healthcare Managers?
Artificial intelligence is likely to change aspects of healthcare management, potentially automating some administrative tasks and providing new tools for data analysis and decision support. However, it's unlikely to eliminate the need for human managers entirely.
AI can augment managers' capabilities, freeing them from routine tasks to focus on more complex strategic issues, leadership, relationship building, and ethical decision-making – areas where human judgment and empathy remain crucial. Managers who adapt and learn to leverage AI tools effectively may find their roles enhanced rather than threatened.
The core responsibilities involving leadership, strategic planning, managing human dynamics, and navigating complex ethical and regulatory landscapes will likely continue to require skilled human managers. Adaptability and a willingness to embrace new technologies will be key.
Are there specific licensing requirements?
Licensing requirements for healthcare managers vary significantly by role and location. General healthcare management roles often do not require a specific license beyond educational qualifications. However, administrators of certain facility types, particularly nursing homes, are licensed in all U.S. states.
Requirements for nursing home administrator licensure typically include meeting specific educational and experience criteria and passing a licensing examination. Some states may have specific requirements for administrators in other types of facilities as well.
It's essential to check the specific licensing regulations in the state or country where you plan to work, especially if targeting roles in regulated settings like long-term care. Professional organizations like the American College of Healthcare Executives (ACHE) can also provide information on standards and requirements.
These books cover legal and regulatory aspects relevant to healthcare management.
Helpful Resources
For those seeking further information or professional development in healthcare management, several organizations and resources are available:
- American College of Healthcare Executives (ACHE): A major professional society offering networking, education, career resources, and the FACHE credential. (ache.org)
- Medical Group Management Association (MGMA): Focuses on practice management, providing resources for managers in physician practices and ambulatory care settings. (mgma.com)
- Healthcare Financial Management Association (HFMA): Specializes in healthcare finance, offering certifications and resources for financial managers in healthcare. (hfma.org)
- U.S. Bureau of Labor Statistics (BLS): Provides detailed information on job outlook, salary data, and work environment for Medical and Health Services Managers. (bls.gov)
- Agency for Healthcare Research and Quality (AHRQ): A U.S. government agency offering research, data, and tools related to healthcare quality, safety, and efficiency. (ahrq.gov)
Navigating a career in healthcare management offers a path to making a significant impact on healthcare delivery and patient well-being. It requires a blend of business acumen, leadership skills, and a deep understanding of the complex healthcare environment. With strong growth projected for the field, it presents a promising avenue for dedicated individuals seeking challenging and rewarding careers.