Respiratory Therapist
Exploring a Career as a Respiratory Therapist
Respiratory Therapists are vital healthcare professionals focused on evaluating, treating, and caring for patients with breathing or other cardiopulmonary disorders. They work with people of all ages, from premature infants whose lungs are not fully developed to elderly patients suffering from chronic lung diseases. This career involves a deep understanding of the respiratory system, critical thinking skills, and the ability to operate sophisticated medical equipment.
Working as a Respiratory Therapist can be incredibly rewarding. You play a direct role in improving patients' quality of life, often in critical situations where your expertise can mean the difference between life and death. The field offers diverse work environments and opportunities for specialization, ensuring a dynamic and engaging career path for those passionate about patient care and respiratory health.
What is Respiratory Therapy?
Definition and Scope
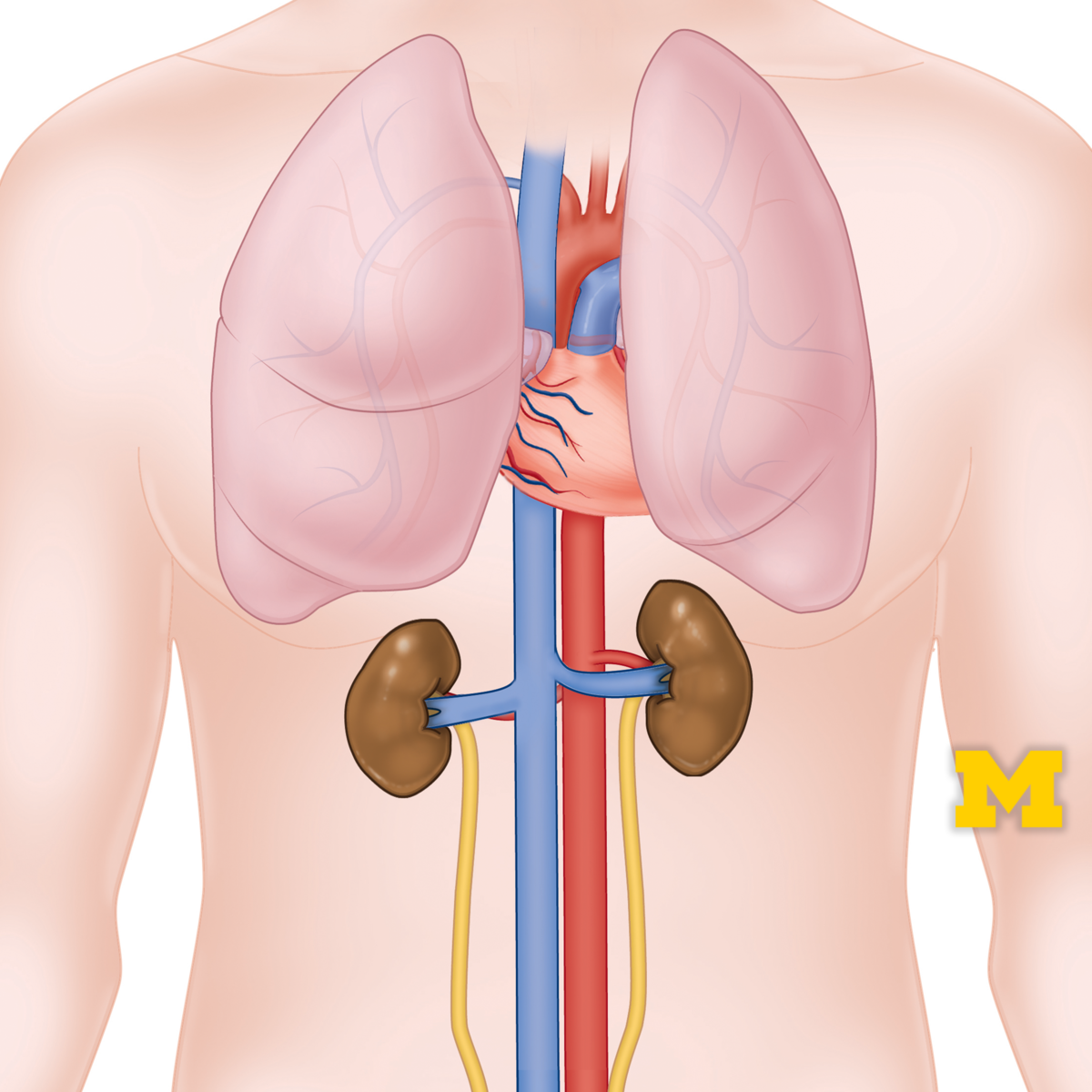
Respiratory Therapy is a specialized healthcare field focused on the assessment, treatment, management, control, diagnostic evaluation, education, and care of patients with deficiencies and abnormalities of the cardiopulmonary system. This system includes the lungs, heart, and associated blood vessels responsible for breathing and circulation.
The scope of practice is broad, ranging from providing emergency care during cardiac arrest or drowning incidents to managing chronic conditions like asthma or emphysema. Respiratory Therapists administer oxygen, manage mechanical ventilators, monitor cardiopulmonary systems, administer medications in aerosol form, and perform diagnostic tests like measuring lung capacity.
They are key members of the healthcare team, collaborating closely with physicians, nurses, and other specialists to develop and implement patient care plans. Their expertise is crucial in various settings, ensuring patients receive appropriate respiratory support and education.
A Brief History
The field of respiratory therapy emerged primarily after World War II, driven by the need to manage respiratory complications from polio epidemics and advancements in oxygen therapy and mechanical ventilation. Initially known as "oxygen technicians" or "inhalation therapists," the role evolved significantly as medical technology and understanding of respiratory physiology advanced.
Formal training programs began to appear in the 1950s and 1960s, establishing standardized education and credentialing. Organizations like the American Association for Respiratory Care (AARC) and the National Board for Respiratory Care (NBRC) were formed to promote professional standards, education, and ethical practice.
Over the decades, the profession has expanded its scope, incorporating sophisticated diagnostic techniques, advanced ventilator management, and specialized care for neonatal, pediatric, and adult populations. Today, Respiratory Therapists are recognized as essential experts in cardiopulmonary care.
Core Responsibilities in Healthcare
A Respiratory Therapist's primary responsibility is to help patients breathe easier. This involves a wide range of tasks tailored to individual patient needs. They assess patient conditions, develop treatment plans, and administer therapies.
Key duties often include managing life support equipment like mechanical ventilators, administering aerosolized medications, performing chest physiotherapy to clear lung secretions, and monitoring oxygen levels. They also conduct pulmonary function tests to diagnose respiratory disorders.
Patient education is another critical component. Therapists teach patients and their families about lung diseases, breathing techniques, and the proper use of respiratory equipment, empowering them to manage their conditions effectively, especially in cases of chronic illness.
These courses provide foundational knowledge in human anatomy and physiology, crucial for understanding the cardiopulmonary system.
Understanding the basics of breathing is fundamental to this field.
Where Respiratory Therapists Work
Respiratory Therapists practice in diverse settings. The most common environment is acute care hospitals, particularly in intensive care units (ICUs), emergency departments, and neonatal/pediatric units where critical respiratory support is often needed.
Beyond hospitals, therapists work in skilled nursing facilities, long-term acute care centers, and rehabilitation clinics, managing patients with chronic respiratory conditions or those recovering from acute illness. Home healthcare is another growing area, allowing therapists to provide care and support in patients' homes.
Some Respiratory Therapists work in diagnostic laboratories performing pulmonary function testing or sleep studies. Others may find roles in physician offices, educational institutions teaching future therapists, or in equipment sales and support for medical device companies.
This course covers vital signs, which are fundamental measurements in patient assessment across various healthcare settings.
Understanding vital signs is a core skill for healthcare professionals.
A Day in the Life: Roles and Responsibilities
Clinical Tasks and Procedures
The daily work of a Respiratory Therapist involves a blend of technical skills, patient assessment, and critical thinking. A significant portion of their time, especially in hospital settings, may involve managing patients on mechanical ventilators. This includes setting up ventilators, adjusting settings based on patient response and blood gas analysis, and troubleshooting equipment issues.
Therapists administer various respiratory treatments, such as inhaled medications via nebulizers or inhalers, chest physiotherapy techniques like percussion and vibration to help clear mucus, and oxygen therapy using different delivery devices. They also perform diagnostic procedures like arterial blood gas sampling and analysis, spirometry, and other pulmonary function tests.
Documentation is also a key part of the role. Respiratory Therapists meticulously record patient assessments, treatments administered, patient responses, and any changes to the care plan in the electronic health record, ensuring clear communication within the healthcare team.
These resources offer insights into pulmonary physiology and the principles of mechanical ventilation, core knowledge areas for RTs.
Gas exchange is a fundamental physiological process managed by RTs.
Responding in Critical Care
Respiratory Therapists are indispensable members of the critical care team, especially during emergencies. They respond to "code blue" situations (cardiac or respiratory arrest), where they are primarily responsible for establishing and maintaining a patient's airway, often through endotracheal intubation, and managing manual or mechanical ventilation.
In the ICU, they manage complex respiratory scenarios, including acute respiratory distress syndrome (ARDS), severe pneumonia, or trauma affecting the lungs. Their expertise in airway management and ventilator strategies is critical for patient survival and recovery.
They must remain calm under pressure, make rapid decisions based on changing patient conditions, and work seamlessly with physicians and nurses during high-stress events. This requires strong technical skills, adaptability, and excellent communication.
These courses cover emergency medical responses, including airway management and critical care interventions.
Understanding intubation and airway management is crucial in critical care.
Patient Education and Chronic Disease Support
Beyond acute and critical care, Respiratory Therapists play a significant role in managing chronic respiratory diseases like Chronic Obstructive Pulmonary Disease (COPD), asthma, and cystic fibrosis. A key aspect of this is patient education.
Therapists teach patients how to use medications and equipment correctly (e.g., inhalers, home oxygen, CPAP machines for sleep apnea). They also educate patients on breathing exercises, smoking cessation strategies, and lifestyle modifications to manage their condition and improve their quality of life.
In outpatient clinics or pulmonary rehabilitation programs, RTs help patients build exercise tolerance and learn self-management skills. This ongoing support empowers patients to take an active role in their health and reduce hospital readmissions.
This course focuses specifically on chronic respiratory diseases like Asthma and COPD.
Understanding specific conditions like asthma and pneumonia is important.
Team Collaboration
Respiratory Therapy is inherently collaborative. Therapists work side-by-side with a diverse team of healthcare professionals. Collaboration with physicians, especially pulmonologists and critical care specialists, is essential for diagnosing conditions and formulating treatment plans.
They also work closely with Registered Nurses to coordinate patient care, monitor patient status, and administer treatments. Communication with other specialists like cardiologists, neonatologists, anesthesiologists, and physical therapists is common, depending on the patient's condition and setting.
Effective teamwork requires clear communication, mutual respect, and a shared understanding of roles and responsibilities. Respiratory Therapists contribute their specialized knowledge of cardiopulmonary function and therapy, ensuring comprehensive patient care.
This course focuses on interprofessional collaboration in healthcare settings.
Working effectively with other healthcare roles is key.
Areas of Specialization
While many Respiratory Therapists work as generalists, there are opportunities to specialize in specific areas of practice. Common specializations require additional experience, education, and often advanced certifications.
Neonatal/Pediatric Respiratory Care focuses on newborns and children with respiratory issues, requiring specific skills for managing tiny airways and unique conditions. Pulmonary Function Technology involves performing complex diagnostic tests of lung function. Sleep Disorders Specialists (often working as Polysomnographic Technologists) diagnose and treat sleep-related breathing disorders like sleep apnea.
Other areas include critical care (requiring the ACCS credential), pulmonary rehabilitation, home care, and adult critical care. Some therapists pursue roles in education, research, or management within healthcare organizations.
These books delve into specialized areas like pediatric care and ICU therapy.
Educational Pathways to Respiratory Therapy
Degree Requirements: Associate vs. Bachelor's
To become a Respiratory Therapist in the United States, the minimum educational requirement is typically an Associate's degree from a program accredited by the Commission on Accreditation for Respiratory Care (CoARC). Many therapists enter the field with an Associate of Science (AS) or Associate of Applied Science (AAS) degree.
However, there is a growing trend towards Bachelor of Science (BS) degrees in Respiratory Therapy. A BS degree often provides a broader education, including more coursework in advanced clinical practice, research methods, leadership, and education, potentially opening more doors for career advancement.
Choosing between an associate's and bachelor's program depends on individual career goals, time commitment, and financial resources. While an associate's degree provides the entry point, a bachelor's degree may be preferred or required for supervisory, management, or educational roles.
Accreditation and Certification
Graduating from a CoARC-accredited program is crucial, as it is a prerequisite for taking the national credentialing exams administered by the National Board for Respiratory Care (NBRC). Accreditation ensures the program meets high educational standards.
After graduation, individuals must pass the NBRC's Therapist Multiple-Choice (TMC) Examination. Achieving a high cut score on the TMC exam makes graduates eligible to take the Clinical Simulation Examination (CSE). Passing both exams earns the Registered Respiratory Therapist (RRT) credential, which is the standard certification for practice.
Virtually all states require Respiratory Therapists to be licensed, and the RRT credential is typically required for licensure. It's essential to check the specific licensing requirements of the state where you intend to practice. You can find more information on accreditation and credentialing through CoARC and the NBRC.
Understanding healthcare education standards is part of the journey.
The Importance of Clinical Internships
Clinical internships, also known as clinical rotations or practicums, are a mandatory and essential component of any accredited respiratory therapy program. These experiences provide students with hands-on practice in real healthcare settings under the supervision of experienced RRTs.
During internships, students apply the knowledge learned in the classroom to actual patient care situations. They gain experience with various types of equipment, procedures, patient populations (adult, pediatric, neonatal), and work environments (ICU, emergency room, general wards, clinics).
These practical experiences are vital for developing clinical competence, critical thinking skills, and professional behavior. They also help students network and often serve as a bridge to employment upon graduation.
This course helps understand clinical terminology often encountered during internships.
Clinical assessment skills are honed during internships.
Continuing Education and Lifelong Learning
The field of respiratory care is constantly evolving with new technologies, treatments, and research findings. Therefore, lifelong learning is essential for maintaining competence and staying current.
Most state licensing boards and the NBRC require Respiratory Therapists to complete a certain number of continuing education units (CEUs) periodically to maintain their license and credentials. These CEUs can be earned through workshops, seminars, conferences, online courses, and other approved educational activities.
Beyond mandatory requirements, pursuing advanced knowledge and skills through continuing education can lead to specialization, career growth, and enhanced patient care. Platforms like OpenCourser offer access to courses covering relevant topics, helping professionals stay updated.
Advancing Your Career in Respiratory Therapy
Starting Your Career: Entry-Level Roles
Upon earning the RRT credential and state licensure, most new graduates begin their careers as staff Respiratory Therapists in hospitals. These entry-level positions provide broad exposure to various aspects of respiratory care, allowing new therapists to solidify their skills and gain experience.
Typical responsibilities include performing routine therapies, managing ventilators under supervision, responding to rapid response calls, conducting basic diagnostic tests, and charting patient care. New graduates often undergo an orientation period working closely with preceptors or senior therapists.
This initial phase is crucial for building confidence and competence across different clinical areas, laying the foundation for future specialization or advancement within the field.
Pursuing Advanced Certifications
For therapists seeking to specialize or demonstrate advanced expertise, the NBRC offers several specialty credentials beyond the RRT. These certifications often require additional experience and passing a separate examination.
Common advanced certifications include the Adult Critical Care Specialist (ACCS), Neonatal/Pediatric Specialist (NPS), and Sleep Disorders Specialist (SDS). Earning these credentials can enhance job prospects, potentially lead to higher salaries, and signify a high level of expertise in a specific area of respiratory care.
These advanced certifications validate specialized skills and knowledge, making therapists valuable assets in critical care, neonatal/pediatric units, or sleep labs.
This handbook provides comprehensive information relevant to general and advanced respiratory care.
Moving into Leadership and Education
Experienced Respiratory Therapists with strong clinical and interpersonal skills may advance into leadership or educational roles. Opportunities exist for positions such as lead therapist, clinical supervisor, or department manager.
These roles involve overseeing staff, managing department operations, ensuring quality care, developing protocols, and handling administrative tasks. Strong leadership, communication, and organizational skills are essential. Often, a Bachelor's or even a Master's degree may be preferred or required for management positions.
Alternatively, therapists passionate about teaching can become clinical instructors in respiratory therapy programs or provide staff education within healthcare facilities. These roles require excellent clinical knowledge and the ability to effectively mentor and educate others.
Transitions to Broader Healthcare Roles
The skills and experience gained as a Respiratory Therapist can also serve as a foundation for transitioning into other roles within the broader healthcare industry. Some therapists pursue further education to move into healthcare administration or management.
Other potential pathways include roles in clinical research, medical device sales or clinical support, patient advocacy, or public health. The clinical knowledge, understanding of healthcare systems, and patient care experience are valuable assets in these related fields.
Exploring these options often requires additional education or certifications specific to the desired role, but the core competencies developed as an RT provide a strong starting point.
This handbook offers insights into healthcare research, a potential transition area.
The healthcare industry offers diverse career paths.
Technological Frontiers in Respiratory Care
Innovations in Mechanical Ventilation
Mechanical ventilation remains a cornerstone of critical care respiratory therapy. Technology in this area continues to advance, focusing on improving patient comfort, safety, and outcomes. Newer ventilators incorporate sophisticated modes that adapt to patient breathing efforts, potentially reducing sedation needs and weaning times.
Features like advanced monitoring graphics, automated adjustments based on physiological targets (like oxygen saturation or end-tidal carbon dioxide), and non-invasive ventilation (NIV) interfaces are becoming more refined. Research explores closed-loop systems that could further automate ventilator management.
Respiratory Therapists must continually update their knowledge and skills to effectively utilize these advanced technologies, ensuring optimal patient care and safety while managing complex machinery.
Telemedicine and Remote Monitoring
Telemedicine is increasingly impacting respiratory care, particularly for managing chronic conditions and providing consultations remotely. Telehealth platforms allow therapists to monitor patients' conditions at home using connected devices like pulse oximeters, spirometers, or even remotely adjustable CPAP machines.
Virtual visits enable patient education, follow-up assessments, and troubleshooting of equipment issues without requiring an in-person appointment. This improves access to care, especially for patients in rural areas or those with mobility limitations.
As telehealth technology evolves, Respiratory Therapists will likely play a larger role in remote patient management, requiring proficiency with digital health tools and virtual communication skills.
These courses discuss telehealth competencies and the role of technology in remote care.
Artificial Intelligence in Pulmonary Diagnostics
Artificial intelligence (AI) is beginning to show promise in enhancing pulmonary diagnostics. AI algorithms are being developed to analyze medical images like chest X-rays and CT scans to help detect conditions like pneumonia, lung nodules, or emphysema with potentially greater speed and accuracy.
AI may also assist in interpreting pulmonary function test results or analyzing data from sleep studies to identify patterns indicative of respiratory disorders. While still evolving, AI tools could augment the diagnostic capabilities of clinicians, including Respiratory Therapists involved in testing.
Therapists may increasingly interact with AI-driven diagnostic tools, requiring an understanding of their capabilities and limitations and how to integrate them into clinical workflows effectively.
This course explores using Azure Health Bot, an example of AI application in healthcare settings.
Advances in Oxygen Delivery
Oxygen therapy is fundamental in respiratory care, and technologies for its delivery continue to improve. Portable oxygen concentrators (POCs) have become smaller, lighter, and more efficient, offering greater mobility and independence for patients requiring long-term oxygen therapy.
Smart oxygen delivery systems are emerging that can automatically adjust oxygen flow based on the patient's real-time needs, detected through sensors monitoring activity levels or oxygen saturation. This aims to optimize oxygenation while conserving oxygen supply.
Respiratory Therapists are key in assessing patients for appropriate oxygen delivery systems, educating them on safe usage, and managing therapy adjustments based on these evolving technologies.
While specific to children, this resource highlights the importance of oxygen therapy.
Ethical Considerations in the Field
Navigating End-of-Life Decisions
Respiratory Therapists are often involved in the care of critically ill patients, placing them at the forefront of complex end-of-life discussions and decisions. Managing life support, such as mechanical ventilation, raises ethical questions about withdrawing or withholding treatment when recovery is unlikely.
Therapists must navigate sensitive conversations with patients, families, and the healthcare team regarding prognosis, patient wishes (advance directives), and the potential burdens versus benefits of continued aggressive care. Respecting patient autonomy while providing compassionate support is paramount.
Understanding ethical principles, communication strategies, and institutional policies surrounding end-of-life care is crucial for navigating these challenging situations professionally and ethically.
Resource Allocation in Critical Settings
In situations like pandemics or mass casualty events, healthcare systems can face shortages of critical resources, including ventilators, ICU beds, and even qualified staff. Respiratory Therapists may be involved in difficult decisions regarding the allocation of these scarce resources.
Ethical frameworks and institutional guidelines aim to ensure fairness and transparency in allocation decisions, but the reality can be ethically distressing for frontline clinicians. Balancing the needs of individual patients with the principles of public health and equitable distribution presents significant challenges.
Understanding triage protocols and the ethical underpinnings of resource allocation helps therapists navigate these high-pressure scenarios, though the moral burden can be substantial.
These resources discuss public health responses and lessons learned from pandemics like COVID-19, which highlighted resource allocation issues.
Balancing Patient Autonomy and Clinical Judgment
Respecting patient autonomy – the right of patients to make informed decisions about their own healthcare – is a fundamental ethical principle. However, situations arise where a patient's decision may conflict with the therapist's clinical judgment about the best course of action.
For example, a patient might refuse a necessary therapy or request a treatment deemed inappropriate or potentially harmful. Therapists must balance respecting the patient's wishes with their professional responsibility to promote well-being and avoid harm.
This requires excellent communication skills to ensure the patient fully understands their condition and treatment options, exploring their values and concerns, and collaborating with the healthcare team to find ethically sound solutions that respect autonomy whenever possible.
Cultural Competency in Treatment
Patients come from diverse cultural backgrounds with varying beliefs, values, and practices related to health, illness, and death. Providing culturally competent care means recognizing and respecting these differences and adapting care delivery accordingly.
Cultural factors can influence communication styles, family involvement in decision-making, acceptance of certain treatments, and perspectives on end-of-life care. Therapists must develop cultural humility and sensitivity to build trust and provide effective, patient-centered care.
This involves being aware of one's own biases, seeking to understand the patient's perspective, utilizing interpreter services when needed, and tailoring education and treatment plans to be culturally appropriate.
Global Perspectives and Opportunities
International Variations in Practice
The practice of respiratory therapy, including educational requirements, scope of practice, and certification or licensure, varies significantly around the world. While the profession is well-established in North America, its development and recognition differ in other regions.
Some countries may have similar roles under different titles or integrate respiratory care tasks into nursing or physiotherapy professions. International standards and recognition agreements are evolving but are not yet universal.
Therapists interested in working abroad must thoroughly research the specific requirements and professional landscape of their target country. This may involve additional education, examinations, or credential evaluation.
These resources offer global perspectives on health issues and systems.
Impact of Global Health Challenges
Global health challenges, such as pandemics (like COVID-19) and deteriorating air quality in many urban areas, significantly impact the demand for and practice of respiratory care worldwide. These events highlight the critical role of respiratory professionals in managing widespread respiratory illness.
Increased prevalence of chronic respiratory diseases linked to environmental factors or lifestyle also drives the need for skilled respiratory care practitioners globally. International collaboration and knowledge sharing become crucial in addressing these shared challenges.
Understanding the global context of respiratory health helps therapists appreciate the broader impact of their profession and potential areas for international contribution or learning.
These courses and books discuss pandemics and infectious diseases from various perspectives.
International Employment Considerations
Opportunities for Respiratory Therapists to work internationally exist, particularly in countries with well-developed healthcare systems or regions experiencing rapid healthcare expansion. However, navigating the process can be complex.
Potential hurdles include credential recognition, language barriers, visa requirements, and adapting to different healthcare systems and cultural norms. Thorough research and preparation are essential.
Networking with international organizations or therapists working abroad can provide valuable insights. Some therapists may find opportunities through volunteer organizations, international health initiatives, or employment with multinational healthcare companies.
Leveraging Online Learning in Respiratory Care
Digital Tools for Skill Enhancement
While hands-on clinical experience is irreplaceable, online learning offers valuable tools for supplementing education and enhancing skills in respiratory care. Digital simulations can provide virtual environments to practice procedures like ventilator setup or airway management in a safe, controlled setting.
Interactive case studies allow learners to apply theoretical knowledge to realistic patient scenarios, developing critical thinking and decision-making abilities. Online modules can also cover specific equipment operation or new treatment protocols.
These digital resources can be particularly useful for students preparing for clinical rotations, graduates studying for credentialing exams, or practicing therapists looking to refine specific skills or learn about new technologies.
Strengthening Foundational Knowledge Online
Online courses are an excellent resource for building or reinforcing the foundational scientific knowledge essential for respiratory therapy. Subjects like anatomy, physiology, pathophysiology, pharmacology, and microbiology form the basis of understanding respiratory diseases and treatments.
Platforms like OpenCourser aggregate courses from various institutions, allowing learners to find resources tailored to their needs. Whether you're a prospective student wanting a head start, a current student needing extra support, or a practitioner needing a refresher, online courses offer flexible and accessible learning options.
You can easily browse health and medicine courses to find relevant materials covering core concepts like gas exchange or cardiovascular function.
These courses cover essential anatomy and physiology concepts, often prerequisites or core components of RT programs.
Continuing Education and Refreshers
Online learning provides a convenient way for practicing Respiratory Therapists to fulfill continuing education requirements and stay current in the field. Many professional organizations and educational platforms offer accredited online courses covering diverse topics.
Online modules can serve as efficient refreshers on specific topics like pharmacology updates, changes in clinical practice guidelines (e.g., for asthma or COPD management), or advanced ventilator modes. This flexibility allows busy professionals to learn at their own pace and on their own schedule.
Keeping knowledge sharp through ongoing online learning ensures therapists continue to provide evidence-based, high-quality patient care throughout their careers.
Understanding the Demands of the Profession
Navigating Shift Work and Schedules
Respiratory care in hospitals is typically a 24/7 necessity, meaning most Respiratory Therapists work shifts, including nights, weekends, and holidays. Common schedules involve 8-hour or 12-hour shifts, which can rotate.
Adjusting to shift work can be challenging, potentially impacting sleep patterns, social life, and overall well-being. Finding strategies to manage irregular schedules, prioritize rest, and maintain a healthy work-life balance is crucial for long-term sustainability in the profession.
While some roles outside of acute care hospitals (e.g., clinics, home care, education) may offer more traditional hours, prospective therapists should be prepared for the demands of shift work, especially early in their careers.
Managing Exposure Risks
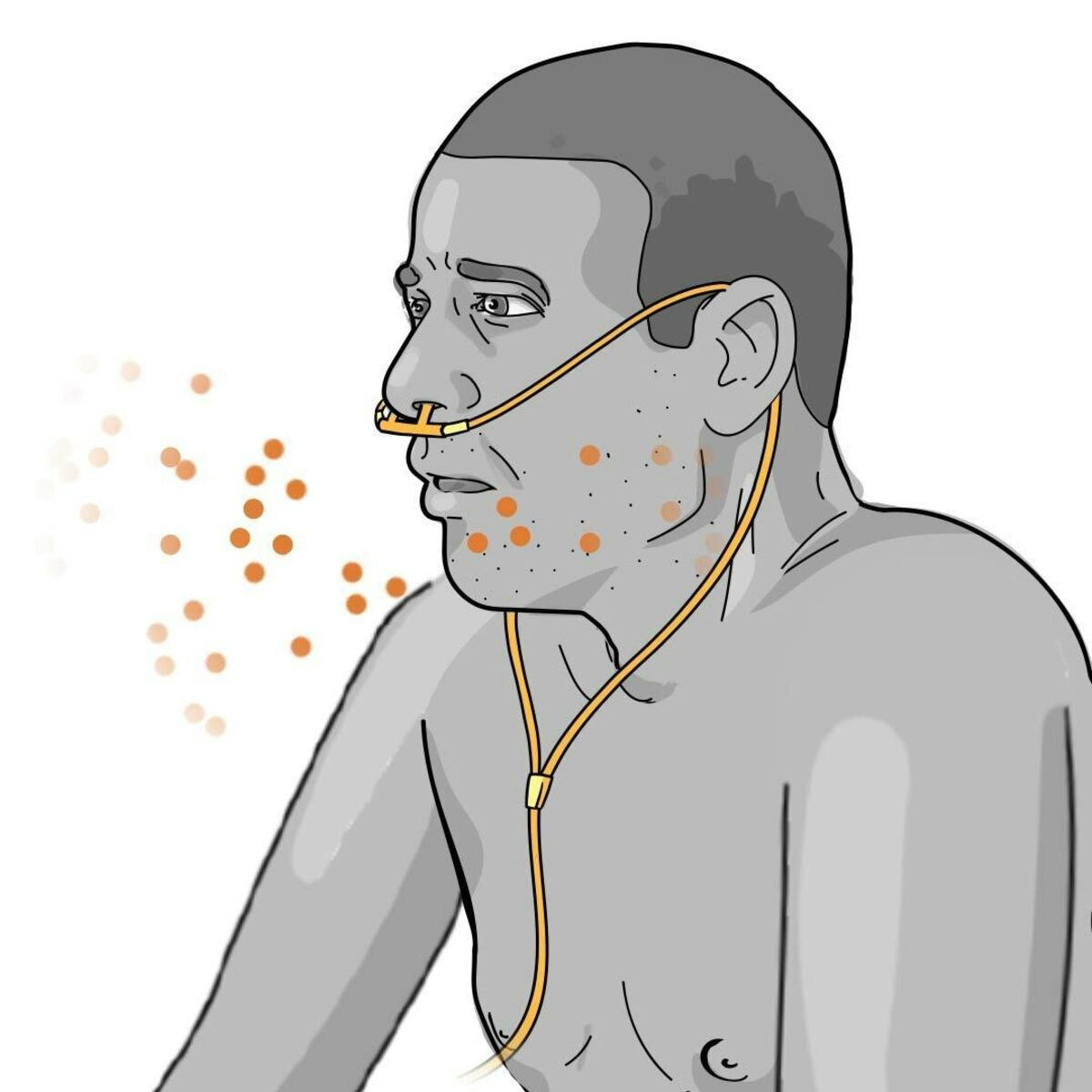
Working closely with patients with respiratory illnesses inherently involves exposure to infectious diseases, including airborne pathogens. Respiratory Therapists perform procedures like suctioning airways or inducing sputum, which can generate aerosols.
Strict adherence to infection control protocols, including proper hand hygiene and the consistent use of personal protective equipment (PPE) like masks, gowns, and gloves, is essential to minimize risk. Healthcare facilities provide training and resources for infection prevention.
While risks exist, following established safety guidelines significantly reduces the likelihood of transmission, protecting both the therapist and their patients. Awareness and diligence are key.
These books cover infectious diseases and public health, relevant to understanding exposure risks.
Coping with High-Stress Environments
Respiratory Therapists frequently work in high-stress environments, particularly in emergency departments and intensive care units. They deal with critically ill patients, life-or-death situations, and rapidly changing conditions that require quick thinking and decisive action.
The emotional toll of witnessing patient suffering, managing complex emergencies, and dealing with loss can be significant. Developing coping mechanisms, stress management techniques, and seeking support from colleagues or mentors is vital.
While challenging, many therapists find deep satisfaction in making a difference during critical moments. However, acknowledging the inherent stress and proactively managing it is essential for mental and emotional health.
This book discusses therapy in the ICU setting, a high-stress environment.
Preventing Burnout
The combination of shift work, exposure risks, high stress, and the emotional demands of patient care can contribute to burnout among Respiratory Therapists. Burnout is characterized by emotional exhaustion, depersonalization, and a reduced sense of personal accomplishment.
Strategies for preventing burnout include maintaining a strong work-life balance, practicing self-care (exercise, hobbies, mindfulness), setting professional boundaries, seeking peer support, and utilizing employee assistance programs if available.
Open communication within the healthcare team and supportive management can also foster a healthier work environment. Recognizing the signs of burnout early and taking proactive steps is crucial for maintaining career longevity and personal well-being.
Ensuring safety and quality improvement can contribute to a better work environment.
Frequently Asked Questions about Respiratory Therapy
What is the typical salary range?
Salary for Respiratory Therapists varies based on factors like geographic location, years of experience, level of education (Associate vs. Bachelor's), credentials (RRT plus specialty certs), work setting (hospital vs. clinic vs. home care), and specific job responsibilities.
According to the U.S. Bureau of Labor Statistics (BLS), the median annual wage for respiratory therapists was $77,960 in May 2023. The job outlook is projected to grow 13 percent from 2022 to 2032, much faster than the average for all occupations. You can find detailed, up-to-date salary and outlook information on the BLS website.
Entry-level salaries will typically be lower than the median, while experienced therapists with advanced credentials or in management roles can earn significantly more. Researching salary data specific to your region and desired work setting is recommended.
Can I advance without direct patient care?
Yes, there are career paths for Respiratory Therapists that involve less direct, hands-on patient care. Experienced therapists can move into roles in management, administration, education, or clinical research.
Positions in healthcare informatics, quality improvement, or patient safety also leverage clinical knowledge without constant bedside care. Additionally, opportunities exist in the medical device industry, working in sales, clinical application support, or product development for respiratory equipment manufacturers.
These roles often require additional education (like a Bachelor's or Master's degree) or specific training, but they offer alternative career trajectories for those seeking different types of professional engagement.
Will automation impact job security?
While technology and automation are advancing in healthcare, the core responsibilities of Respiratory Therapists involve complex clinical judgment, hands-on skills, patient assessment, and interpersonal communication – tasks that are difficult to fully automate.
Technology, like advanced ventilators or AI diagnostics, is more likely to augment the therapist's role rather than replace it. Therapists will need to adapt and learn to utilize new tools effectively. The aging population and prevalence of chronic respiratory diseases suggest continued strong demand for skilled respiratory care professionals.
The hands-on nature of many RT procedures and the need for critical thinking in dynamic patient situations make widespread replacement by automation unlikely in the foreseeable future. Job security is expected to remain robust according to projections like those from the BLS.
Should I specialize or remain a generalist?
The decision to specialize or remain a generalist depends on individual interests, career goals, and the job market in your area. Working as a generalist, especially early in your career, provides broad experience across different patient populations and settings.
Specializing (e.g., in neonatal/pediatrics, critical care, sleep disorders) allows for deeper expertise in a specific area. This can lead to roles in specialized units, potentially higher pay, and recognition as an expert. However, specialization might limit flexibility if job opportunities in that niche are scarce in a particular location.
Many therapists gain general experience first before pursuing advanced certifications and specializing. Consider your long-term interests and research opportunities in your desired geographic area when making this decision.
How did COVID-19 affect the field?
The COVID-19 pandemic significantly highlighted the critical importance of Respiratory Therapists. As the virus primarily attacked the respiratory system, RTs were essential frontline workers managing ventilators, oxygen therapy, and airway support for severely ill patients.
The pandemic increased public awareness of the profession and underscored the need for skilled respiratory care practitioners. It also accelerated the adoption of certain technologies, like telehealth for follow-up care, and reinforced the importance of infection control measures.
While incredibly challenging, the pandemic solidified the vital role of RTs in healthcare, potentially leading to increased respect and demand for the profession long-term. Many courses were developed to address the specifics of COVID-19 care.
These courses were created specifically to address the COVID-19 pandemic, reflecting the field's adaptation.
Are RT skills transferable to other jobs?
Yes, many skills developed as a Respiratory Therapist are highly transferable to other healthcare roles and even some non-healthcare positions. Core competencies include critical thinking, problem-solving, patient assessment, communication, teamwork, technical proficiency with medical equipment, and understanding complex physiological processes.
These skills are valuable in related clinical roles such as nursing (often requiring additional education), cardiovascular technology, or sleep technology. They are also applicable in healthcare education, administration, medical sales, clinical research coordination, and public health.
While direct transition may require further training or certification depending on the target role, the foundational knowledge and practical skills gained in respiratory therapy provide a strong basis for diverse career pathways within and beyond traditional clinical practice.
Consider exploring related healthcare careers available on OpenCourser.
Becoming a Respiratory Therapist is a challenging yet deeply rewarding path for individuals passionate about science, technology, and direct patient care. It requires dedication, continuous learning, resilience, and compassion. If you are drawn to a dynamic healthcare career where you can make a tangible difference in people's ability to breathe, Respiratory Therapy may be an excellent choice for you. Explore resources on how to leverage online learning to build your foundation or supplement your education as you consider this vital profession.